13. Minisymposium „Infektion und Immunabwehr“ Burg
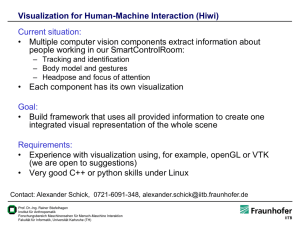
Werbung
13. Minisymposium „Infektion und Immunabwehr“ Burg Rothenfels, 12. – 14. März 2009 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 SCIENTIFIC PROGRAM 13. Minisymposium „Infektion und Immunabwehr“ Burg Rothenfels, 12. – 14. März 2009 PROGRAMM Organisation: C. Hölscher, Borstel D. Schlüter, Magdeburg G. van Zandbergen, Ulm Donnerstag, 12.3.08 14.45 Abfahrt Bus-Shuttle Würzburg Hauptbahnhof (Vorplatz) 15.30 – 16.30 Ankunft, Zimmerverteilung, Kaffee und Gebäck 16.30 – 17.40 Session 1: Signalling and effector molecules Chair: Alexander Dalpke 1 Murine 65 kDa GBPs : important effector molecules in Toxoplasma infection. Daniel Degrandi et al., Düsseldorf 2 Identification of a novel subcellular localization pattern of Suppressor of Cytokine Signalling – 1 (SOCS-1) Julia Strebovsky et al., Heidelberg 3 SOCS-1 enhances Pasteurella multocida Toxin induced STAT3 activity Katharina F. Kubatzky et al., Heidelberg 2 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 4 The role of Frizzled1 in M. tuberculosis infection : Modes of induction and first insights into function Jan Neumann et al., Kiel 5 Wnt ligands differentially regulate the inflammatory response of macrophages upon mycobacterial infection Kolja Schaale et al., Kiel 6 Influence of optineurin on adenovirus E3-14.7K mediated TNF-resistance Wulf Schneider-Brachert et al., Regensburg 7 Downregulation of AP-1 proteins in Chlamydia pneumoniae infected host cells Christiane Jugert et al., Luebeck 17.40-18.00 Pause 18.00 – 19.00 Session 2: T and B cells Chair: Andreas Limmer 1 Delayed type hypersensitivity versus humoral immune response – Influence of high and low antigen doses on the cytokine expression within spleenic compartments Claudia Stamm et al., Luebeck 2 Injury – induced Th cell suppression after injury is restored through targeting dendritic cells in the regenerating tissue Florian Wirsdörfer et al., Essen 3 Apoptotic Leishmania major mediate a Th2 response in BALB/c mice Julia Barthelmann et al., Luebeck 4 Bacterial DRiPs, Yes or No Silke Grauling – Halama et al., Heidelberg 3 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 5 In E.coli Nissle 1917 monocolonized Rag1 deficient mice CD4+ T cells are essential for the protection against dissemination and septic shock Ute Eberle et al., Tuebingen 6 The regulatory T cell response during acute viral infection is locally defined and controls the magnitude and duration of the virus-specific cytotoxic T cell response Kirsten Dietze et al., Essen 19.00 – 20.00 20.00 Abendessen Key note lecture 1 Introduction: Dirk Schlüter Frank Kirchof, Ulm: Mechanisms of HIV-1 immune evasion ab ca. 21 Uhr Chill out Freitag, 13.3.08 9.00 – 10.30 Session 3: TLRs and innate immune responses Chair: Christian Bogdan 1 TLR against R848 inhibits differentiation of mDCs and leads to differentiaton of tolerogenic APc from CD14+ monocytes Sabine Woelfle et al., Heidelberg 2 Improvement of host defense in the lung Thomas Tschernig et al., Hannover 4 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 3 The phosphatidylserine binding protein annexin A5 can interfere with chlamydial infection. Lisa Pfleiderer et al., Ulm 4 Characterization of dual production of IFN-beta and IL12/23 p40 on a single cell basis after TLR stimulation. Magdalena Kocur et al., Düsseldorf 5 Antiretroviral effects of Toll-like receptor ligands Kathrin Gibbert et al., Essen 6 Functional analysis of cells from IFIT-2 knockout mice Alexandra Siegfried et al., Tuebingen 7 The role of cytokines for NK cell activation in visceral leishmaniasis Simone Haeberlein et al., Erlangen 8 Acute treatment against cutaneous leishmaniasis with a two component gel developing nitric oxide Beate Lorenz et al., Mainz 9 The role of Natural killer (NK) T cells for protection against Leishmania major infection Klaus Griewank et al., Mainz 10:30 – 11:00 Kaffeepause 11.00 – 12.30 Session 4a: Cytokines Chair: Stefan Ehlers 1 Tumor-derived Prostaglandin E2 and TGF-beta synergize to inhibit PDCderived IFN-alpha Marijo Parcina et al., Heidelberg 5 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 2 Role of type I IFNs in innate defence to Legionella pneumophila Bastian Opitz Berlin 3 The visualization of IFN-beta producing cells versus their infection state in time course studies during of MCMV infection Stephanie Borkens et al., Duesseldorf 4 Induction of pro-inflammatory IL-!2 in Plasmodium berghei infected BALB/c mice breaks blood-brain-barrier and leads to cerebral malaria Kim Ellen Schmidt et al., Bonn 5 The role of interleukin 22 in Toxoplasma gondii induced ileitis Melba Munoz et al., Berlin 6 The interleukin-13/ interleukin-4 receptor –alpha axis is involved in tuberculosis associated pathology Lisa Heitmann et al., Borstel 7 Blockade of IL-6 trans-signalling does not reactivate experimental tuberculosis Jan Christian Sodenkamp et al., Borstel 8 IL-17 maintains protective immunity during Mycobacterium tuberculosis infection Jochen Behrends et al., Borstel 9 The IL-23 / IL-17 axis is required for protective immune responses against Trypanosoma cruzi infection Hanna Erdmann et al., Borstel 12.30 – 13.30 Mittagessen anschließend Spaziergang und Kaffee 6 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 15.30 – 17.00 Session 4b: Dendritic cells and macrophages Chair: Christoph Hölscher 1 Molecular mechanisms involved in aberrant type 1 interferon-induction by S.aureus protein A. Sibel Durlanik et al., Heidelberg 2 Detrimental role of dendritic cells during Y.enterocolitica infection in vivo Philipp Warnke et al., Tübingen 3 Leishmania amastigote propagation in human host cells Elena Bank et al., Ulm 4 Role of Langerin+ skin-derived DC in Leishmania major infection Kordula Kautz-Neu et al., Mainz 5 Opsonization of L.major with cross-reactive anti-phospholipid antibodies promotes phagocytosis by dendritic cells (DC) and induction of protective immunity Susanna Lopez Kostka et al., Mainz 6 Role of hypoxia and HIF-1 alpa in dendritic cell immunobiology. Jonathan Jantsch et al., Erlangen 7 Conventional and plasmacytoid bone marrow-derived dendritic cells contribute to Toll like receptor-independent IFN-alpha/ beta production in response to inactivated parapoxvirus ovis Gottfried Alber et al., Leipzig 8 Activation of macrophages by the mycobacterial cord factor (TDM) and its synthetic analogue (TDB) Hanne Schoenen et al., Erlangen 7 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 9 Interaction of Mycobacterium tuberculosis and human macrophages under hypoxic conditions. Daniel Nickel et al., Ulm 17.00–17.30 Fachgruppenaktivitäten Ger van Zandbergen, Dirk Vorsitzende der Fachgruppe/des Arbeitskreises 17.30 Schlüter Keynote lecture 2 Introduction: Ger van Zandbergen Freddy Frischknecht, Heidelberg: Imaging motile pathogens ca. 18.30 Uhr Buffet Samstag, 14.3.08 9.00 – 10.10 Session 5a: Immunomodulation Chair: Norbert Reiling 1 Split tolerance after oral vaccination of mice with recombinant Escherichia coli Nissle 1917 expressing fimbrial adhesion K88 Katharina A. Remer et al., Würzburg 2 Acute graft-versus –host-disease after reduced intensity conditioning is mediated by MyD88 mediated TLR9 sensing of bacterial DNA and can be modulated by administration of TLR antagonist. Rita Plickert et al., Berlin 8 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 3 Long –term effect of sepsis –The influence of bacteremia and bacterial translocation on systemic adaptive immune responses Timo Schwandt et al., Bonn 4 Systemic bacterial infection alters differentiation of dendritic cells in the bone marrow and mediates chronic dendritic cell dysfunction. Eva Pastille et al., Essen 5 Increased susceptibility to infection with Aspergillus fumigatus in graft-versushost disease is not due to impaired pathogen clearance Bernd Echtenacher et al., Regensburg 6 Modulation of host macrophage apoptosis by Leishmania infection Stefanie Enzenmüller et al., Ulm 7 Protective effect of filarial infection inhibiting malaria outcome in mice Susanne Deininger et al., Bonn 10.10 – 10.30 Kaffepause 10.30 – 12.00 Session 5b: Organ-specific regulation of immune responses Chair: Gottfried Alber 1 Immune regulatory functions of alveolar type II epithelial cells Dunja Bruder et al Braunschweig 2 Airway epithelial cells modify immune responses Lotte M. Schmidt et al., Heidelberg 3 Corneal inflammation in response to filarial antigens Katrin Gentil et al., Bonn 9 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 4 The contribution of the innate, placental immune system to defend the fetus from infections Diana Friedrich et al., Erlangen 5 A crucial role of the spleen in the induction of pathogenic host responses towards P. berghei ANKA infection Beatrix Schumak et al., Bonn 6 The role of the intestinal microflora in infection with Citrobacter rodentium Ulrich Steinhoff et al., Berlin 7 IL-4/ IL-13-dependent alternative activation of macrophages but not microglial cells is associated with uncontrolled cerebral cryptococcosis Werner Stenzel et al., Berlin 8 Neuron and astrocyte –specific function of IKK-2 and NEMO in Toxoplasma encephalitis Ulrike Händel et al., Magdeburg 9 Toxoplasma gondii induces behavioural changes in infected mice M. Fahad Haroon et al., Magdeburg 12:00 Preisverleihung 12:05 Ende der Tagung Lunchpaket / Mittagessen 13.00 Abfahrt Bus (pünktlichst!) 10 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 ABSTRACTS (in alphabetical order of presenting authors) Conventional and plasmacytoid bone marrow-derived dendritic cells contribute to Toll-like receptor-independent IFN-alpha/beta production in response to inactivated parapoxvirus ovis Sabine Siegemund1, Andrea Hartl2, Franziska Dautel1, Ruediger Raue3, Marina A. Freudenberg4, 2 Mathias Buettner5, Gabriele Koehler6, Carsten J. Kirschning2, Tim 1 Sparwasser , Gottfried Alber 1 Institute of Immunology, College of Veterinary Medicine, University of Leipzig, Germany; 2 Institute of Microbiology, Technische Universitaet Muenchen, Germany; 3 Pfizer Animal 4 Health, Kent, United Kingdom; Max Planck Institute for Immunobiology, Freiburg, Germany; 5 Bayerisches Landesamt für Gesundheit und Lebensmittelsicherheit, Oberschleissheim, Germany; 6 Gerhard-Domagk-Institute for Pathology, Universitaetsklinikum Muenster, Germany Parapoxvirus ovis (PPVO) is a member of the Poxviridae family and belongs to the genus Parapoxvirus. It displays only limited homology with orthopoxviruses and has some molecular features such as an unusual high GC content distinct from orthopoxviruses. Inactivated parapoxvirus ovis (iPPVO) has strong immunostimulatory capacities mediating antiviral activity in vivo. The role of dendritic cells and the pattern recognition receptors responsible for recognition of iPPVO are unknown. We demonstrate that bone marrowderived plasmacytoid dendritic cells (BM-pDC) and bone marrow-derived conventional dendritic cells (BM-cDC) secrete IFN-alpha/beta in response to iPPVO. Furthermore, iPPVO induces TNF-alpha and IL-12/23p40 release and MHC-II, MHC-I and CD86 up-regulation by bone marrow-derived dendritic cells (BMDC). After engulfment, iPPVO was located in endosomal compartments and in the cytosol of BMDC. Although iPPVO is a double-stranded DNA virus, the DNA-recognizing toll-like receptor (TLR) 9 is not involved in iPPVO-induced release of IFN-alpha/beta by BMDC. Moreover, we demonstrate that iPPVO elicits IFNalpha/beta by TLR-independent pathways, since IFN-alpha/beta release does not require myeloid differentiation primary response gene 88 (MyD88) or TIR-domain containing adaptor protein inducing interferon (TRIF). In contrast, iPPVO-induced TNF-alpha and IL-12/23p40 release and enhanced expression of MHC-I and CD86 but not MHC-II by BMDC partially depends on MyD88 but not on TLR2, TLR4 or TLR9. These results provide first evidence that iPPVO mediates its immunostimulatory properties by TLR-independent and -dependent pathways and demonstrate an important role of cDC for IFN-alpha/beta production. 11 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Leishmania amastigote propagation in human host cells Elena Bank 1, Alexander Wenzel1 and Ger van Zandbergen1. 1 Instiute for Medical Microbiology and Hygiene, University Clinic of Ulm Leishmania major (L. major) is an obligate intracellular parasite elegantly misusing the apoptotic cell clearance system for disease development. This parasite enters polymorphonuclear neutrophil granulocytes (PMN) in its promastigote form. Hiding inside Annexin A5 (AnxA5)-positive PMN the parasite transfers into macrophages (MF), where it multiplies in its amastigote form. We found that the presence of AnxA5-binding population of promastigotes is responsible for the survival and infectivity of viable promastigotes inside PMN. Still relatively little is known about macrophage infection by the amastigote form of L. major propagating the disease. We developed a novel in vitro method to culture the amastigote form of L. major and compared these amastigotes with promastigotes We found them to be higly infectious for different types of human MF. To study amastigote development and propagation in more detail, we generated eGFP expressing L. major. The eGFP marker is upregulated in the amastigotes stage. Using these transfectants we infected type I (inflammatory) and typ II (anti-inflammatory) human MF. We found that type II MF take up more parasites as compared to type I MF. Using FACS analyses we could detect the development of amastigotes by a higher expression level of eGFP as compared to the eGFP expression of intraphagocytic promastigotes. Focussing on amastigote uptake using timelapse imaging we found that dying eGFP-negative and AnxA5-positive amastigotes enter MF first followed by viable eGFP-positive parasites. These new tools will enable us to examine L. major amastigote propagation in human host cells. 12 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Apoptotic Leishmania major mediate a Th2 response in BALB/c mice Julia Barthelmann, Juergen Westermann, Kathrin Kalies Institute of Anatomy, University of Luebeck It has recently been reported that the virulent inoculum of Leishmania major (L. major) promastigotes conventionally used for infection experiments contains about 50% of apoptotic parasites. The depletion of apoptotic parasites lead to a reduced infectivity in BALB/c mice in vivo. In order to analyse the detrimental effect of apoptotic leishmania on the immune response in the lymph node, we separated viable and apoptotic L. major by magnetic cell separation. We studied T-cell proliferation and cytokine mRNA expression in the draining lymph node after infection of susceptible BALB/c mice with viable L. major. We found that the lack of apoptotic parasites in the inoculum leads to a delay of disease progression and decreased IL-4 and IL-10 mRNA levels 6 weeks after infection, while IFN-gamma levels remain unchanged. Furthermore, Th2-associated total serum IgG1 levels are reduced. Disease, cytokine mRNA production and total serum IgG1 after 6 weeks could be restored by adding apoptotic leishmania to the inoculum, thereby indicating that apoptotic L. major support the establishment of a Th2 immune response. Although the initial composition of the inoculum determines the disease development, the response in the lymph node is not defined 3 days after infection: Time point and magnitude of initial T-cell proliferation do not differ compared to conventional L. major infections and the cytokine pattern does not correlate with the final disease outcome. Overall, the removal of apoptotic parasites in the inoculum decreases the Th2 response, but does not explicitly support the establishment of a Th1 phenotype in susceptible BALB/c. 13 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 IL-17 maintains protective immunity during Mycobacterium tuberculosis infection Jochen Behrends,1 Dominik Rueckerl,1 Manuela Heßmann,1 Uwe Mueller,2 Gottfried Alber,2 Yoichiro Iwakura,3 Stefan Ehlers4,5 & Christoph Hoelscher1 1 Infection Immunology, Research Center Borstel, Germany; 2University of Leipzig, Germany; 3 University of Tokyo, Japan; 4Microbial Inflammation Research, Research Center Borstel, Germany; 5Molecular Inflammation Medicine, Christian-Albrechts-University, Kiel, Germany Because a variety of autoimmune disorders have now been shown to depend on interleukin (IL)-17-producing T helper (TH)17 cells, therapeutic blockade of TH17 development may provide a novel approach to avoid adverse consequences of anti-inflammatory strategies such as reactivation of latent tuberculosis (TB). To evaluate the potential risk of interfering with IL-17-dependent inflammation, we analyzed the outcome of experimental TB in IL-17deficient (-/-) mice after infection with Mycobacterium tuberculosis (Mtb). IL-17 was important for the induction of neutrophil chemokines after Mtb infection, but was not involved in granuloma formation and protection during the first three months of Mtb infection. Mtbinfected IL-17-/- mice efficiently generated interferon-gamma (IFN)-producing T cells and IFNgamma-dependent effector responses. However, IL-17-/- mice were not able to control mycobacterial replication during the chronic phase of experimental TB and died significantly earlier than corresponding wildtype mice. This breakdown of immune protection in IL-17-/mice was associated with a drop in the frequency of IFN-producing CD4+ T cells. Our findings reveal that IL-17 is essential for maintaining CD4+ T cell-dependent protection during chronic stages of TB. Hence, interfering with IL-17-dependent pathways as an antiinflammatory therapeutic approach will possibly incur the danger of reactivating latent TB. (Supported by the Inflammation Research Excellence Cluster) 14 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The visualization of IFN-beta producing cells versus their infection state in time course studies during of MCMV infection Stephanie Borkens1, Vu Thuy Khanh Le2, Stefanie Scheu1 1 Institute of Medical Microbiology and Hospital Hygiene, University of Duesseldorf 2 Institute of Virology, University of Duesseldorf Type I interferons are a family of multiple IFN-alphas and a single IFN-beta which were initially identified on the basis of their antiviral activities. Previous findings identified pDCs as the major IFN-beta producing cells in the spleen. However, which cells are actually infected with MCMV remains unclear, although it has been suggested that at certain stages of infection MCMV can actively replicate in macrophages and conventional DCs. For a detailed analysis of the initial phase of MCMV infection, we used a MCMV strain which expresses EGFP under the immediate-early promoter (MIEP) to infect IFN-beta/YFP reporter knockin mice. This experimental approach allows for the simultaneous visualization of the IFN-beta response and the infection status of MCMV in vivo. In initial analyses at 24h post infection. we identified splenic pDCs as well as few CD11b+ cells expressing IFN-beta. Furthermore, we could show that the IFN-beta producing pDCs are not directly infected with MCMV and that mainly CD11b+/c+ cells expressed EGFP as a marker for MCMV infection. Current studies aim at the clarification of IFN-beta-production versus the infection status of individual cells in this simultaneous analysis during several time points of infection. 15 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Immune regulatory functions of alveolar type II epithelial cells Marcus Gereke, Harro Frauendorf, Dunja Bruder Immune regulation group, Helmholtz Center for Infection Research, Braunschweig Whereas the lung epithelium was long time related primarily with physical barrier and gas exchange functions, the contribution of alveolar type II epithelial cells (AECII) in respiratory immune regulation has become increasingly appreciated. However, their precise function in the induction and regulation of T cell reactivity to self antigen remains poorly understood. Utilizing a transgenic mouse model for CD4+ T cell mediated pulmonary inflammation we found that MHC class II expressing AECII present self-antigen to CD4+ T cells resulting in functional activation of lung-reactive T cells and finally autoimmunity. Importantly, we unravelled a previously unknown immunological attribute of AECII in re-establishment of peripheral T cell tolerance in the lung. Upon inflammation, AECII secrete a broad variety of soluble factors including transforming growth factor-beta (TGF-beta), Platelet Factor-4 and Surfactant Protein-A and -D, which suppress T cell proliferation and induce in a partially TGF-beta dependent mechanism Foxp3 expression in lung-reactive CD4+ T cells. As a part of the innate immune system AECII thus exhibit so far underestimated immune regulatory function and synergize with adaptive immune mechanisms to re-establish tolerance to selfantigen in the lung. Preliminary data suggest that upon influenza infection alveolar self antigen recognition by CD4+ T cells does not result in increased abundance of Foxp3 expressing regulatory T cells thus indicating that the capability to respond to and to eradicate a pathogen dominates about the necessity to protect against potentially harmful autoimmune reactions. Currently we are investigating the contribution of AECII in balancing tolerogenic and pathogen-specific immunity in the lung. 16 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Murine 65 kDa GBPs: important effector molecules in Toxoplasma infection. Daniel Degrandi, Carolin Konermann, Cornelia Beuter-Gunia, Sarah Lahme, Anna Fischer, Elisabeth Kravets, Klaus Pfeffer Medizinische Mikrobiologie und Krankenhaushygiene. Heinrich-Heine-Universität Düsseldorf The 65 kDa guanylate-binding proteins comprise a growing family of highly conserved GTPases, found in mice, humans, and many other species. In mice, 11 members of the GBP family have been described. In recent studies, we could show that several members of the mGBP family colocalize with the parasitophorous vacuole (PV) of avirulent Toxoplasma gondii (Tg) strains, suggesting a direct antiparasitic function of the mGBP proteins. Interestingly, highly virulent Tg strains are able to modulate the cellular response to the infection and suppress the recruitment of mGBP proteins to the PV. The mechanisms involved in the recruitment of mGBP proteins to the PV and their molecular and biochemical activity are the major focus of our current studies. First results indicate, that GTP-binding and hydrolysis are needed for normal localization of the proteins in infected and uninfected cells. Furthermore, the recruitment of mGBP proteins towards the Toxoplasma PV is dependent on the microtubular network, since cells treated with Paclitaxel and other microtubule interacting drugs showed no colocalization of mGBPs with the PV. Studies in mGBP2-/- mice showed an increased susceptibility towards infections with Tg. Also, mGBP2 deficient cells show a significantly reduced capability to control Tg growth in vitro. These data indicate, that the family of 65 kDa mGBPs play crucial roles in the cell autonomous defense against intracellular pathogens. 17 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Protective effect of filarial infection inhibiting malaria outcome in mice Susanne Deininger1, Daniel Fernández-Ruiz1, Gwydion Brennan1, Bettina Dubben1, Achim Hoerauf1, Sabine Specht1 1 Institute for Medical Microbiology, Immunology and Parasitology, University Hospital Bonn, Bonn, Germany Malaria is a serious tropical disease with a high risk of mortality to date. Chronic helminth infections and often co-endemic with malaria and both might alter the immune response against another. By use of a co-infection model of the filarial nematode Litomosoides sigmodontis and the malaria pathogen Plasmodium berghei ANKA in Balb/c mice we discovered that a preceding filarial infection inhibited a subsequent infection with P. berghei sporozoites in one-third of mice. Interestingly, this sterile protection was correlated with presence of microfilariae, which are the first stage larvae of the filarial parasite. We observed increased levels of activated T cells in spleen and liver of microfilaremic mice. Furthermore, phagocytotic cells were increased in the spleens of these mice. In order to investigate the underlying mechanism, we analysed cytokine profiles in these mice. We found that worminfected mice produced higher levels of IL-10, IFN-gamma and granzyme B and their CD4+ and CD8+ T cells were found to be in an activated status (CD69+) secreting IFN-gamma, perforin and granzyme B. Both candidates the cytotoxic T cells and the phagocytotic cells may contribute to the mechanisms responsible for blocking parasitaemia of malaria pathogens in a part of filarialinfected mice. A better knowledge about the protective mode of a patent filarial infection on the outcome on malaria may provide some tools to influence the course of malaria in favour for the host. 18 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The regulatory T cell response during acute viral infection is locally defined and controls the magnitude and duration of the virus-specific cytotoxic T cell response Kirsten Dietze1, Gennadiy Zelinskyy1, Ulf Dittmer1 1 Institut fuer Virologie, Universitaetsklinikum Essen Cytotoxic T-cells (CTL) facilitate control of acute viremia in many viral infections, including retroviruses like HIV or HTLV. However, viruses that establish chronic infections have developed mechanisms to evade destruction by CTL. We have used the Friend Virus (FV) model to investigate these mechanisms. In the acute infection FV induces a strong CTL response but the mice become persistently infected. However, regulatory CD4+ T cells (Treg) that expand in the spleen of infected mice suppress the production of cytotoxic molecules in CD8+ T cells and the cytotoxic function of CTL. The aim of our current work was to analyse the compartmentalisation of the Treg response and the subsequent local suppression of CD8+ T cells by Tregs during an ongoing retroviral infection. We found, that expansion of effector CD8+ T cells, production of cytotoxic molecules and degranulation was directly linked to viral loads in lymphatic organs. Consequently the expansion of induced Treg correlated with the number and function of virus-specific CD8+ T cells. For the expansion of Treg the presence of CTL was obligatory, what was shown by CD8 depletion experiments. Furthermore, depleting Treg in DEREG mice resulted in enhanced expansion of effector CD8+ T cells and improved the production of cytotoxic molecules leading to reduced viral loads in lymphatic organs. In summary, during acute retroviral infection Treg downregulated the expansion and function of virus-specific CTL. The immunosuppressive activity of Tregs was locally defined to the organs in which efficient viral replication followed by a strong CD8+ effector cell response took place. 19 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Molecular mechanisms involved in aberrant type I interferon-induction by S. aureus protein A Isabelle Bekeredjian-Ding1, Sibel Durlanik1, Marijo Parcina1, Sandra Ammann1, Wulf Schneider-Brachert2 Klaus Heeg1 1 Hygiene-Institute, Dept. of Med. Microbiology and Hygiene, UniversityHospital Heidelberg 2 Institute for Med. Microbiology und Hygiene, University of Regensburg Protein A (SpA), an immunoglobulin (Ig)-binding protein, is a major virulence factor of Staphylococcus aureus and well-known as an immunostimulatory protein. We previously observed that certain strains of S. aureus induce IFN-alpha secretion from plasmacytoid dendritic cells (pDC). The aim of the project presented was therefore, to investigate the role of SpA in type I interferon induction from pDC. Remarkably, IFN-a induction correlated with bacterial levels of SpA expression, and subsequent experiments showed that recombinant SpA induces IFN-alpha secretion from pDC. Moreover, IFN-I induction could be blocked by saturating Ig or Fc fragments, indicating that the Ig-binding domain may be essential for IFN-I induction. Most importantly, DNAse and RNAse digestion of recombinant SpA did not alter its ability to induce IFN-I. Recently, SpA has been shown to bind TNFR1 on respiratory epithelial cells. Here we show that anti-TNF-R mAb neutralisation can inhibit the SpAinduced type I interferon secretion. We further show that SpA colocalizes with the TNF-R2 in transfected HEK293 cells. Thus, SpA may represent a novel TLR-independent stimulus for pDC activation. 20 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 In E. coli Nissle 1917 monocolonized Rag1 deficient mice CD4+ T cells are essential for the protection against dissemination and septic shock. Ute Eberle* 1, Kerstin Fink*1, Martina Müller1, Frank Leithäuser2, Thomas A. Ölschläger3, Ingo B. Autenrieth1, Julia-Stefanie Frick1 1 Institute of Medical Microbiology and Hygiene, University of Tuebingen, Germany 2 Institute of Pathology University of Ulm, Germany 3 Institute of Molecular Biology of Infection, University of Wuerzburg, Germany * equal contribution E. coli Nissle 1917 (EcN) is a well defined probiotic E. coli strain, which is effective in maintaining remission in ulcerative colitis. The aim of this study was to explore safety aspects of this frequently used probiotic strain. Therefore, germfree Rag1-/- mice were monocolonized with EcN. Upon CD4+ T cell transfer germfree Rag1-/- mice showed a high mortality rate due to dissemination of EcN. In peripheral organs high bacterial loads of EcN were detected correlated with high levels of TNF in the serum. In contrast, SPF Rag1-/- mice colonized with EcN showed no dissemination of EcN in peripheral organs even though the numbers of bacteria in the intestine did not differ. Furthermore, EcN monocolonized C57Bl/6 mice showed no increased mortality rate, indicating that CD4+ T cells were essential either for the inhibition of translocation or for the clearance of EcN from the peripheral organs. The translocation and dissemination are an EcN specific effect, as it was not observed in germfree Rag1-/- mice monocolonized with E. coli mpk, a commensal E. coli stain isolated from the murine intestine. Additionally, the dissemination of EcN in monocolonized Rag1-/mice was not flagella dependent. As the translocation of EcN Dflic and DflgE to peripheral organs was comparable to the translocation of wildtype EcN. Therefore, an unknown bacterial factor seems to account for the dissemination of EcN in monocolonized Rag1-/mice, and both the immature intestinal barrier and the immature mucosa associated immune system of germfree animals seem to be essential for the translocation of EcN. 21 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Increased susceptibility to infection with Aspergillus fumigatus in graft-versus-host disease is not due to impaired pathogen clearance Bernd Echtenacher1, Kristina Doser 2, Matthias Edinger2 and Petra Hoffmann2 1 Institute of Immunology, University Regensburg and 2 Dept. of Hematology and Oncology, University Hospital Regensburg, Regensburg, Germany Graft-versus-host disease (GvHD) is a frequent and life-threatening complication after allogeneic bone marrow transplantation (alloBMT) that is initiated by mature alloreactive T cells within the graft. These show excessive proliferation and pro-inflammatory cytokine secretion upon interaction with host antigen-presenting cells, which leads to a dysregulated cytokine milieu and finally results in tissue damage and target organ destruction (gut, liver and skin). Patients after alloBMT are severely immunocompromised and therefore particularly prone to opportunistic bacterial and fungal infections. While immunosuppressive medication for GVHD prophylaxis clearly raises the risk of infection, the contribution of GVHD itself to this increased susceptibility is much less understood. To evaluate the impact of GVHD on the host's defence against fungal infections, allo-transplanted BALB/c mice with or without GVHD were infected intratracheally or intravenously with the clinically relevant pathogen Aspergillus fumigatus. Mortality was significantly higher in GVHD animals (only 20% survival after 2wks) as compared to the non-GVHD group (75% survival for more than 5wks). Interestingly, clearance of the fungus from the lung after i.t. infection, or from spleen and liver after i.v. infection, was rapid and comparable in both groups and no live fungus was detectable in moribund animals. However, when lymphocytes isolated from spleen and liver of infected animals were restimulated in vitro with germinating conidia, cells from GVHD animals secreted significantly more pro-inflammatory TNF and IL-6 than those from control mice. This suggests that an uncontrolled inflammatory immune response contributes to the high morbidity and mortality of opportunistic infections in GVHD. 22 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Modulation of host macrophage apoptosis by leishmania infection Stefanie Enzenmüller1, Cordula Schropp2, Simone Fulda1, Ger van Zandbergen2 and Silke Fischer1,2 1 University Children's Hospital, Ulm. 2 Institute for Medical Microbiology and Hygiene, University Clinic of Ulm Leishmania are obligate intracellular parasites which undergo a promastigote flagellated stage in the sandfly and an aflagellated amastigote stage in vertebrate hosts. They cause a spectrum of human diseases, ranging from self-limiting cutaneous infections to visceral leishmaniasis. The infection of mammalian hosts is initiated by promastigotes that are phagocytosed by macrophages either directly or after infection of neutrophils initially recruited to the sandfly bite. In host cells Leishmania replicate and differentiate to amastigotes. Like all intracellular parasites, Leishmania have evolved specialized strategies to evade immune destruction and to interact with multiple apoptotic systems to complete their life cycle. The repression of host cell apoptosis is one type of strategy to protect the host macrophage in which the intracellular parasites replicate and persist. Our main research interest is focused on how Leishmania major interferes with the host cell apoptotic machinery in infected cells. Therefore we investigate how Leishmania modulate the different signalling pathways of apoptosis. We used two different cell lines (monocyte-derived macrophages THP1 and murine macrophage-like Raw 264.7). Cells were infected with L. major in vitro and subsequently treated with external apoptosis-inducing stimuli such as UVlight or staurosporine. First results are indicating that L. major inhibits caspase activation, cytochrome c release from mitochondria and modulates the level of BH3-only proteins within the infected macrophage cells. 23 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The IL-23/IL-17 axis is required for protective immune responses against Trypanosoma cruzi infection Hanna Erdmann,1 Caroline Rossnagel,1 Nico Ghilardi,2 Yoichiro Iwakura,3 Thomas Jacobs,4 Christoph Hoelscher1 1 Infection Immunology, Research Center Borstel, Germany; Francisco CA USA; 3 2 Genentech, South San Center for Experimental Medicine, Institute of Medical Science, University of Tokyo, Japan; 4Bernhard-Nocht-Institute for Tropical Medicine and Hygiene, Hamburg, Germany Interleukin (IL)-12 is a potent inducer of interferon-gamma (IFN)-producing T helper (TH)1 cells and promotes a protective cell-mediated immune response after infection with the protozoan parasite Trypanosoma cruzi, the causative agent of Chagas disease. IL-23 is structurally closely related to IL-12 and shares the IL-12/23p40 subunit and the corresponding IL-12 receptor 1 subunit. However, IL-23 is not as potent as an inducer of IFN-production than IL-12. Instead IL-23, but not IL-12, promotes the proliferation of IL-17producing TH17 cells. To analyze the role of IL-23 for protective immune responses during experimental Chagas disease, IL-23p19 deficient (-/-) mice were infected with T. cruzi. Compared to wild-type mice, IL-23p19-/- mice developed a higher parasitemia and an increased mortality. However, this susceptibility was not due to an impaired TH1 immune response. Because IL-23 supports the development of IL-17-secreting TH17 cells, we infected IL-17-/- mice with T. cruzi to study the relevance of IL-17 for protective immune responses. Like IL-23-/- mice, IL-17-/- mice exhibited a higher parasitemia, an elevated mortality and an altered liver pathology. Moreover, TH1 immune responses were not affected by the absence of endogenous IL-17. Together, we suggest here that in addition to TH1 cells, IL-23-dependent TH17 cells are required for a successful resolution of T. cruzi infection. One important effector cytokine that mediates this IFN-independent arm of the protective immune response during experimental Chagas disease appears to be IL-17. Downstream effector mechanisms induced by IL-17 are currently under investigation. (Supported by the Inflammation Research Excellence Cluster). 24 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The contribution of the innate, placental immune system to defend the fetus from infections Diana Friedrich, André Gessner, Daniela Klaffenbach, Jörg Dötsch, and Markus Schnare Institut für Mikrobiologie - Klinische Mikrobiologie, Immunologie und Hygiene des Universitätsklinikums Erlangen, Wasserturmstr. 3-5, 91054 Erlangen The placenta establishes an anatomical barrier between the maternal side and the developing fetus. Nevertheless, it is a potential origin where pathogens coming from the maternal tissue might traverse to the fetal itssue. Therefore, we hypothesized that the placenta upon pathogen encounter is able to orchestrate an immune response by releasing inflammatory chemokines and cytokines. Furthermore the placenta might be able to express a broad repertoire of antimicrobial effector proteins to directly fight against the incoming bacterial threat. The stimulation of isolated placental cells with TLR-ligands or complete bacteria enhanced the secretion of the chemokine IL-8, the proinflammatory cytokines IL-6 and TNF as well as the anti-inflammatory cytokine IL-10 in a stimulus dependent manner. In addition purified placental cells expressed the antimicrobial effector proteins bactericidal/permeabilityincreasing (BPI), beta-defensin 2, secretory leucocyte protease inhibitor and acyloxyacyl hydrolase. Group B streptococci were potent stimulators of these products. Because the synthesized spectrum of AMPs and cytokines identified from isolated placenta cells is similar to what can be observed from neutrophilic granulocytes, we separated trophoblasts from lymphocytes by MACS. Indeed by flow cytometry we could demonstrate that granulocytes were present in the isolated trophoblast fraction. After the separation no lymphocytes could be detected in the purified cell fraction. Via confocal scanning laser microscopy we were able to detect intracellular expression of BPI in purified trophoblasts. This separation step will enable us to determine the specific contribution of the purified trophoblasts and the associated hematopoietic cells for the expression of the cytokines or antimicrobial effector proteins. 25 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Corneal inflammation in response to filarial antigens Katrin Gentil1, Eric Pearlman2, Achim Hoerauf1 1 Institute for Medical Microbiology, Immunology and Parasitology, University Clinic Bonn 2 Department of Ophthalmology and Center for Global Health and Diseases, Case Western Reserve University, Cleveland, OH, USA River blindness caused by the filarial nematode Onchocerca volvulus is the second leading cause of blindness in the developing world. Infections with O. volvulus cause corneal inflammation eventually leading to sclerosing keratitis and blindness. Our group has been using a mouse model of filarial infection to investigate the mechanisms of neutrophil migration to the cornea. We were investigating the role of Toll-like receptors (TLRs) in the generation of adaptive immune responses and migration of granulocytes to the corneal stroma. We found decreased IFNgamma production by splenocytes of immunized TLR2-/- mice when compared with immunized C57BL/6 mice. Similarly, we found decreased CXC chemokine production in the cornea and decreased neutrophil infiltration into the corneal stroma in TLR2-/- mice. In contrast, IL-5 production and eosinophil migration were unaffected in TLR2-/- mice. Further analysis revealed decreased neutrophil migration in IFNgamma-/- mice. We could demonstrate that IFNgamma primes macrophages for activation by filarial extracts by upregulation of TLR2 expression on the cell surface leading to increased production of proinflammatory cytokines. These in turn induce CXC chemokine production by corneal fibroblasts that attract neutrophil migration to the cornea. These findings demonstrate that although parasites typically induce strong Th2 responses, the low levels of Th1 responses present during filarial infection are potent inducers of neutrophil migration and corneal inflammation. 26 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Antiretroviral effects of Toll-like receptor ligands Kathrin Gibbert1, Ulf Dittmer1 1 Institut für Virologie; Universitaetsklinikum Essen The Toll-like receptor (TLR) system plays an important role in the recognition of infectious pathogens and their signals induce the coordinated activation of innate and adaptive immune response. Nothing was known about the simultaneous activation of the TLR 3, 7 and 9 ligands which induce various cytokines like Type I Interferons or Interleukin-12 in acute retroviral infection. In the current study, we analyzed the expression of inflammatory cytokines by BM-derived DCs stimulated with different combinations of TLR ligands. A simultaneous incubation with the TLR 3 ligand Poly I:C and the TLR 7 ligand Resiquimod (R848) led to a stronger induction of IL-12 compared to the stimulation with just one of those ligands. We used the Friend retrovirus model to get more insight into the role of the combined TLR ligand stimulation in an acute retroviral infection. Treatment of FV-infected mice with Poly I:C and R848 alone or in combination led to a strong reduction in viral loads in the blood and the spleen. An expansion of NK cells and a strong activation of B cells was found in the TLR ligand treated animals. We could show that the depletion of CD8+ T cells in Poly I:C-treated, FV-infected animals led to an increase of viral loads in the spleen and the bone marrow whereas the depletion of NK cells resulted in higher viral loads in the bone marrow but not in the spleen. In summary Poly I:C and R848 showed a very strong antiviral activity in vivo. Thus, the use of TLR ligands with strong antiviral activity might be a good feature for the treatment of retroviral infections. 27 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Bacterial DRiPs, Yes or No? Silke Grauling-Halama and Gernot Geginat Institut für Medizinische Mikrobiologie und Hygiene, Fakultät für Medizin Mannheim der Universität Heidelberg, Theodor-Kutzer-Ufer 1-3, 68167 Mannheim The rapid recognition of infected cells by CD8 T cells requires fast processing of pathogenderived antigens in the cytoplasm of the host cell followed by subsequent presentation of antigenic peptides in the context of MHC class I molecules on the surface of infected cells. A still unsolved paradox is the discrepancy between a rather long half-live of antigens in the presence of rapid presentation of pathogen-derived antigenic peptides. Studies with virally infected cells suggest that instable structurally altered, so-called defective ribosomal products “DRiPs” are the main source of antigen in infected cells. As viral DRiPs can’t be studied independent of host cells we took advantage of the facultative intracellular bacterium Listeria monocytogenes which enabled us to characterize T cell antigens in infected cells as well as independent of host cells. Our data indicate that similar to virally infected cells the rapid processing of L. monocytogenes derived T cell antigens also depends on an instable form of antigen. In contrast to viral DRiPs, however, the instable form of antigen is not defined by structural alterations of antigens but is a temporary state that antigens are exposed to in their statu nascendi. In summary, our studies suggest a general antigen processing model that does not necessitate the assumption of defective protein synthesis as basis of rapid antigen processing and presentation of stable T cell antigens. 28 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The role of Natural killer (NK) T cells for protection against Leishmania major infection Klaus Griewank, Beate Lorenz, Michael Fischer, Susanna Lopez Kostka, Esther von StebutBorschitz Dept of Dermatology, Johannes Gutenberg-University, Mainz Leishmaniasis is a serious disease affecting 12 million people worldwide and causing tens of thousands of deaths every year. Infection with Leishmania is also a classic immunological model with resistant mouse strains developing Th1 immunity and susceptible strains initiating a Th2 response leading to failure to contain the infection and eventually death. Here we studied the influence of NKT cells on the development of immunity against L. major using a physiological low dose infection model. Our initial results showed that NKT cell-deficient (CD1d-/- or Ja18-/-) C57BL/6 mice were better able to contain Leishmania infections than their wildtype counterparts. Lesions and parasite burdens in CD1d-/- mice were at least 2fold smaller than in C57BL/6 mice (lesions ~2-fold difference wk3, 5 and 8, p<0.05 to 0.0001, parasite burden ear wk5 p<0.05). Application of 100 ng of the NKT cell stimulating glycolipid alpha-Galactosyl-Ceramide (aGalCer) led to a more severe course of disease in C57BL/6 mice associated with higher parasite burdens in infected lesions and spleens (>10 fold; p<0.1 ear, p<0.05 spleen). In contrast, aGalCer administration to susceptible BALB/c mice improved their ability to contain Leishmania infections as measured by differences in lesion sizes and parasite burdens (5–fold; p< 0.05 wk5 and 8). In summary, our findings show that in low dose infections with L. major, NKT cells can alter the immune response against Leishmania, most likely by influencing the cytokine milieu early on. Modulating NKT cell responses, for instance with glycolipid ligands, could be a successful approach to develop a long awaited vaccine against this important human pathogen. 29 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The role of cytokines for NK cell activation in visceral leishmaniasis Simone Haeberlein, Heidi Sebald, Ulrike Schleicher and Christian Bogdan Microbiology Institute - Clinical Microbiology, Immunology and Hygiene; University Clinic of Erlangen, Wasserturmstraße 3-5, 91054 Erlangen The innate immune response in C57BL/6 mice infected with the intracellular protozoan parasite Leishmania (L.) infantum, an agent of visceral leishmaniasis, is characterized by the stimulation of natural killer (NK) cells. NK cells activated in vivo show enhanced cytotoxic activity and secrete interferon (IFN)-gamma which is crucial to induce production of Ieishmanicidal nitric oxide by infected macrophages. We previously demonstrated that the activation of NK cells in L. infantum-infected mice requires the presence of myeloid dendritic cells that are able to phagocytose the parasites and sense them by toll-like receptor 9. This stimulates the production of interleukin (IL)-12, which was shown to be essential for the induction of NK cell effector functions, whereas type I interferons were dispensable. In our ongoing studies we now identified IL-18 as an additional signal for NK cell activation during L. infantum infection. The IFN-gamma secretion and the anti-tumor cytotoxic activity of splenic NK cells from infected C57BL/6 IL-18-/- mice was significantly reduced compared to wild-type controls. Surprisingly, the degranulation of NK cells measured by CD107a surface expression, which is assumed to correlate positively with cytotoxicity, was in fact increased in IL18-/- mice, despite the decreased cytolytic activity in the chromium-release assay. In conclusion, priming of NK cells by IL-18 is crucial to achieve full NK cell activation in L. infantum-infected mice. Subsequent work will further investigate the differential effects of IL18 and analyse whether additional cytokines such as IL-15 are also involved in the process of NK cell activation in experimental leishmaniasis. 30 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Neuron- and astrocyte-specific function of IKK-2 and NEMO in Toxoplasma encephalitis Ulrike Händel,1 Martina Deckert,2 Dirk Schlüter 1 Institut für Medizinische Mikrobiologie, OvG Universität Magdeburg, 39120 Magdeburg, Germany; 2 Abteilung für Neuropathologie, Universität zu Köln, 50937 Köln, Germany; The obligate intracellular parasite Toxoplasma gondii induces a chronic persisting encephalitis and is controlled by T and B cells. Although T. gondii infects brain resident cells including astrocytes, neurons and microglia, the function of these cells in Toxoplasma encephalitis (TE) is much less well defined compared to T and B cells. Since the transcription factor NF-B is a major regulator of immune responses and intracellular survival of T. gondii may be dependent on a manipultation of the NF-kB pathway, we studied the role of neuronal and astrocytic IKK-2 and NEMO, two members of the NF-kB signalling cascade, in TE. After infection of mice deficient in neuronal or astrocytic expression of IKK-2 and NEMO, respectively, with T. gondii, all mouse strains developed a TE with only slight differences in survival and parasite control as compared to control mice. However, neuronal loss was more pronounced in inflammatory lesions of mice with neuronal deletion of IKK2. In addition, cultured primary IKK2-deficient neurons exhibited an increased cell death after infection with T. gondii as compared to neurons from control mice. These findings suggest that IKK-2 is important for an optimal survival of neurons in TE but that a topographally restricted loss of neurons close to inflammatory infiltrates does not result in an increased mortality. 31 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Toxoplasma gondii induces behavioural changes in infected mice. M. Fahad Haroon1, F. Angenstein4, H. Lison2, W. Wetzel2, J. Goldschmidt3, H. Scheich2, E. Budinger2, D. Schlüter1 1 Institute of Medical Microbiology, Universitätsklinikum Magdeburg, Leipziger Straße 44, 39120 Magdeburg 2 Department Auditory Learning and Speech, Leibniz Institute for Neurobiology (IfN), Brenneckestraße 6, 39118 Magdeburg 3 Special Laboratory Non-invasive Brain Imaging, Leibniz Institute for Neurobiology (IfN), Brenneckestraße 6, 39118 Magdeburg 4 Special Laboratory Behavioural Pharmacology, Leibniz Institute for Neurobiology (IfN), Brenneckestraße 6, 39118 Magdeburg It has been previously reported that Toxoplasma gondii-infected mice exhibit an altered behaviour and loose their natural fear of cat urine. However, it is unclear whether these behavioural changes are due to (i) infection of brain areas important for behaviour, e.g. amygdala, (ii) active alteration of neuronal functions by the parasite or (iii) the ensuing immune response. To address these questions we infected BALB/c mice with T. gondii cysts (DX strain) and analysed these animals at days 30 and 60 pi. MRI and histology depicted large, randomly distributed inflammatory lesions in the infected mice without any predilection for brain areas modulating behaviour. These findings suggest that a preferential anatomical location of parasite-induced inflammation is not responsible for behavioural changes of mice. Immunohistochemistry showed that T. gondii infected mainly glial cells and neurons and that T. gondii cysts persisted in neurons. Interestingly, cyst harbouring neurons had frequently axonal contact to non-infected neurons and both, the axon and the non-infected neuron, stained positive for amorphous T. gondii antigen. This may suggest that the persisting obligate intracellular parasite might actively influence the neuronal activity of non-infected neurons. Furthermore, thallium uptake experiment revealed that cyst harbouring neurons showed no dynamic influx of potassium, which indicates that they were electrically silent and functionally inactive. This might additionally contribute to an altered neuronal activity and behavioural changes of mice. 32 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The interleukin-13/interleukin-4 receptor-alpha axis is involved in tuberculosisassociated pathology Lisa Heitmann,1 Tanja Schreiber,1 Thorsten Thye,2 Andrew N. J. Mckenzie,3 Frank Brombacher,4 Rolf D. Horstmann,2 Christian G. Meyer,2 Stefan Ehlers,5,6 & Christoph Hoelscher1 1 Infection Immunology, Research Center Borstel, Germany; 2Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany; 3MRC Laboratory of Molecular Biology, Cambridge, UK; 4University of Cape Town, South Africa; 5Molecular Inflammation Medicine, Research Center Borstel, Germany; 6Molecular Inflammation Medicine, Christian-Albrechts-University, Kiel, Germany. Reactivation and granuloma necrosis (GN) are pivotal events of post-primary tuberculosis (TB). To date, there is no clear evidence whether interleukin (IL)-4 and IL-13 are involved in the pathogenesis of the disease. Therefore, we genotyped polymorphisms in IL-4, IL-13 and the IL-4 receptor alpha-chain (IL-4R) in patients with pulmonary TB from Ghana. A structural variant of the IL-4R, which has been shown to be associated with an increased transcription of the gene, was found to be significantly associated with increased cavity size indicating a prominent role of the IL-4R in human GN. In Mtb-infected mice, however, IL-4 and IL-13 are only moderately induced and necrotizing granulomas are not apparent. To address the question how IL-4R-mediated mechanisms affect the outcome of murine TB, IL-13-overexpressing (IL-13tg) mice were infected with Mycobacterium tuberculosis (Mtb). Aerosol infection of IL-13tg mice resulted in a profound induction of arginases concomitant with increased bacterial loads at chronic stages of the disease very much resembling reactivation TB. Importantly, in IL-13tg mice Mtb infection resulted in tissue pathology similar to GN in human TB. From our data we conclude that IL-4R-dependent mechanisms are involved in the pathogenesis of post-primary TB. (Supported by a BMBF Collaborative Grant and the Inflammation Research Excellence Cluster). 33 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Role of hypoxia and HIF-1alpha in dendritic cell immunobiology Jonathan Jantsch1, Johannes Schödel2, Melanie Volke1,2 , Nadine Turza3, Ulrike Schleicher1, Alexander Steinkasserer3, Christian Bogdan1, Markus Schnare 1, Carsten Willam 2 1 Microbiology Institute – Clinical Microbiology, Immunology and Hygiene, 2Department of Nephrology and Hypertension, and 3 Department of Dermatology, University Hospital Erlangen, Friedrich-Alexander University of Erlangen-Nuremberg, Erlangen, Germany Dendritic cells play a key role in linking innate and adaptive immunity. In inflamed tissues oxygen tensions are thought to be low. The role of hypoxia and of the key player of hypoxic gene regulation, the transcription factor hypoxia inducible factor 1alpha (HIF-1 alpha), are largely unkown. Therefore, we investigated the effects of hypoxia and HIF-1alpha on murine DC activation and function in the presence or absence of lipopolysaccharide (LPS). Hypoxia alone did not activate murine DC, whereas hypoxia combined with LPS led to augmented DC activation compared with LPS alone. Interestingly even under normoxic conditions, DC activation was accompanied by accumulation of HIF-1alphaprotein levels, induction of glycolytic HIF target genes, and enhanced glycolytic activity. Predominantly, this LPS induced stabilisation of HIF-1alpha under normoxic conditions relies on a MyD88dependent NF-kappaB activity. Using RNA interference techniques, knockdown of HIF-1alpha significantly reduced glucose use in DC, inhibited their maturation, and led to an impaired capacity of DC to stimulate allogeneic T cells. Altogether, our data indicate that HIF-1 alpha and hypoxia play a crucial role for DC activation in inflammatory states. 34 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Downregulation of AP-1 proteins in Chlamydia pneumoniae infected host cells Christiane Jugert1, Matthias Klinger2, Werner Solbach1, Ger van Zandbergen3, Jan Rupp1 1 Institut für Med. Mikrobiologie und Hygiene, Ratzeburger Allee 160, 23538 Luebeck 2 Institut für Anatomie, Ratzeburger Allee 160, 23538 Luebeck 3 Institut für Med. Mikrobiologie und Hygiene, Albert-Einstein-Allee 11, 89081 Ulm The development of Chlamydia pneumoniae (Cp) depends on the regulation of cell type specific transcription factors of the host cells. The protein families of the transcription factor AP-1 are known to determine cell life and death in response to extracellular stimuli. Chlamydia-infected host cells are resistant to apoptosis induced by a wide spectrum of proapoptotic stimuli. Our work focuses on the regulation of AP-1 proteins in Chlamydia infected host cells. HEp2-cells were infected with Cp for up to 72 hours. Nuclear proteins were extracted and the DNA binding activity of AP-1 was measured by EMSA. To analyse the expression of different AP-1 proteins, Western blot analysis were performed. Whereas AP-1 activity was upregulated in Cp infected HEp2-cells in the early phase of the developmental cycle, AP-1 proteins were downregulated in the late phase. Degradation of c-Jun protein could also be shown in a degradation assay with cell extracts. The overexpression of c-Jun through transient transfection resulted in smaller inclusion bodies and lower recovery indicating that down regulation of c-Jun is necessary for rapid development of Cp. Summing up, our data indicate that AP-1 proteins are differentially regulated in early and late stages of Cp infected HEp2-cells. We assume that Cp downregulates the expression of AP-1 proteins through degradation to inhibit host cell apoptosis and to fulfil its developmental cycle. 35 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Role of Langerin+ skin-derived DC in Leishmania major infections Kordula Kautz-Neu1, Madelon Noordegraaf2,3, Stephanie Dinges 1, Clare L. Bennett2,4, Björn E. Clausen2,3, Esther von Stebut1 1 Dept. of Dermatology, Johannes-Gutenberg University, 55131 Mainz, Germany; 2Dept. of Cell Biology and Histology, Academic Medical Center, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; 3Dept. of Immunology, Erasmus University Medical Center, 3015 GE Rotterdam, The Netherlands; 4Dept. of Haematology, University College London, Royal Free Hospital, London, NW3 2PF, United Kingdom Langerhans cells (LC) constitute a unique subset of dendritic cells (DC) in the epidermis. These DC are characterized by the expression of MHCII, CD11c and Langerin. In addition to LC, the skin contains a second type of Langerin+ DC, the Langerin+ dermal DC (dDC). Epidermal LC and Langerin+ dDC migrate to skin draining lymph nodes under both steady state and inflammatory conditions. The exact DC subtype responsible for the induction of protective immunity against L. major has not been identified so far. In this study we analyzed the role of Langerin+ skin-derived DC in the physiologically relevant low dose Leishmania infection model. We utilized a diphtheria toxin (DT)-based system that allows the inducible in vivo ablation of Langerin+ cells. In knock-in mice expressing a DT receptor (DTR) cDNA under the control of the Langerin gene (Langerin-DTR mice) the entire population of epidermal LC was eliminated 48 h after a single injection of DT. Interestingly, in low-dose infections with L. major (1x103 parasites), DT-treated Langerin-DTR mice developed significantly smaller lesions, increased IFNgamma/IL-4 ratios and decreased parasite loads compared to control mice. Since repopulation of skin with dDC is much faster than with LC, selective depletion of LC only showed that LC, not dDC, were responsible for this effect. In re-infection experiments, no difference was observed between DT- and PBS treatment suggesting that Langerin+ skin-derived DC are not required for development of an intact memory response. Interestingly, the number of CD4+ Foxp3+ regulatory T cells (Treg) in infected ears was reduced in DT-treated Langerin-DTR mice in comparison to control mice. In contrast to prior studies, our data clearly reveal a suppressive role of epidermal LC in the course of L. major infection via induction of Treg, as the depletion of these cells leads to a better disease outcome. 36 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Characterization of dual production of IFN-beta and IL12/23 p40 on a single cell basis after TLR stimulation Magdalena Kocur1, Stefanie Scheu1 1 Institute of Medical Microbiology and Hospital Hygiene, Heinrich-Heine-University Düsseldorf Type I Interferons and IL-12/23 p40 play important roles in the response to bacterial and viral infections and link innate and adaptive immunity. Their expression is activated in response to TLR ligand binding mainly on antigen presenting cells. It has been shown that IFN-beta contributes to the regulation of p40 expression, but data concerning its possible negative or positive effect remain controversial. To determine the localization and kinetics of the production of these cytokines in vivo, a double reporter mouse system for IFN-beta/YFP and IL12/23 p40/GFP was established. Previous findings showed that after injection of the TLR9 ligand CpG in vivo IFN-beta is mainly expressed in plasmacytoid dendritic cells, but to a very low extent additionally by conventional dendritic cells. For the expression of IL12/23 p40 only the in vivo expression after injection of the TLR4 ligand LPS was determined to be restricted to conventional dendritic cells until now. Here we characterize phenotypically cells, which show dual versus single expression of IFN-beta and IL12/23 p40 after systemic stimulation with several TLR-ligands. In vitro analysis of GM-CSF DCs will determine a possible co- or counterregulation of both cytokines after TLR stimulation in individual cells. The characterization of the effect of combined versus single TLR stimulation is facilitated by the analysis of the frequency of secreted cytokine amounts by ELISA versus quantification of cytokine producing cells as identified by the respective reporter allele. 37 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 SOCS-1 enhances PASTEURELLA MULTOCIDA Toxin induced STAT3 activity Dagmar Hildebrand, Klaus Heeg and Katharina F. Kubatzky Hygiene Institute, Dept. of Hygiene and Medical Microbiology, Im Neuenheimer Feld 324, 69120 Heidelberg Pasteurella multocida Toxin (PMT) is a mitogenic protein toxin that causes respiratory diseases in wild and domestic animals. PMT is able to perturb mammalian signalling cascades through activation of heterotrimeric G proteins and downstream signalling events. Recently we showed that PMT induces signal transducers and activators of transcription (STAT) activity through Galphaq mediated activation of Janus kinases (JAK). Activation of the JAK-STAT pathway is persistent, as PMT does not induce expression of suppressor of cytokine signalling (SOCS) proteins. Overexpression of SOCS-1 in HEK293 cells, however, did not decrease STAT3 activity, but enhanced it significantly. SOCS proteins also act as E3 ubiquitin ligases that target proteins, such as JAKs, to proteasomal degradation. Function as an E3 ligase, however, is dependent on the phosphorylation status of SOCS-1 and serine phosphorylation of SOCS-1 was shown to abrogate proteasomal degradation. We therefore determined the expression levels of the tyrosine kinase JAK2 and found them to be elevated in the presence of SOCS-1, eventually causing hyperphosphorylation of JAK2 and STAT3. The serine/threonine kinases of the Pim family are STAT dependent genes and the protein was shown to interact with SOCS-1 previously. Stimulation of cells with PMT induced expression of Pim-1 that accumulated over time. In addition, we found that SOCS-1 is heavily threonine phosphorylated after PMTstimulation but not after stimulation with IL-6. We hypothesise that persistent expression of Pim-1 leads to phosphorylation of SOCS-1 which protects JAK2 from proteasomal degradation. JAK2 accumulates, leading to hyperactivation of STAT3 and enhanced transforming potential. 38 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Opsonization of L. major with cross-reactive anti-phospholipid antibodies promotes phagocytosis by dendritic cells (DC) and induction of protective immunity Susanna Lopez Kostka, J. Hurst1, Filiz Demircik2, Philipp von Landenberg1, Mark C. Udey3, Ari Waisman2, and Esther von Stebut. Department of Dermatology, 1Institute of Clinical Chemistry and Laboratory Medicine, 21st Medical Department, Johannes Gutenberg-University Mainz, Germany, and 3Dermatology Branch, NCI, NIH, Bethesda, USA. DC acquire L. major through FcgR/IgG-mediated phagocytosis. Thus, both B cell- and Fcgdeficient mice were more susceptible to leishmaniasis which was directly attributable to a failure of DC to prime T cells efficiently and to reduced production of IFNg. We now investigated how initial B cell responses to the parasite itself develop. L. major parasites display phospholipids on their surface. Here, parasites were opsonised by incubation with normal mouse serum (NMS), immune serum (IS) from infected mice or serum containing anti-phospholipid IgG (PhAk-S). Binding of Ab to Leishmania was detected by FACS. Second, both IS as well as PhAk-S significantly enhanced phagocytosis of L. major by DC as compared to unopsonized controls or NMS (35±5 and 27±5% vs. 13±1 and 18±3% infected DC, n5). Next, mice were infected with parasites opsonised with NMS, IS or PhAk-S. Both Leishmania-specific IgG (IS) as well as cross-reactive PhAk-S significantly improved disease outcome. Finally, genetically modified C57BL/6 mice which produce membrane-only IgM+ B cells and have no immunoglobulins (“IgMi”) displayed increased susceptibility as compared to wild type mice. Interestingly, the IgMi phenoptye was normalized upon reconstitution with NMS, but if IS was used for adoptive transfer, the mice showed a significantly improved disease outcome (smaller lesions/faster resolution). In conclusion, our findings suggest that cross-reactive antibodies are found in NMS which bind to pathogens to facilitate phagocytosis of L. major leading to DC-/IL-12-mediated induction of protective immunity. Prior B cell-priming does not seem to be absolutely required to facilitate clearance of this important human pathogen in vivo. 39 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Treatment against cutaneous leishmaniasis with a two component gel developing nitric oxide Beate Lorenz, Alfred Goldinger1, and Esther von Stebut. Department of Dermatology, and 1Central Pharmacy, Johannes Gutenberg-University Mainz, Germany. Nitric oxide (NO) released by e.g. activated MF exerts powerful effects against L. major. We have now investigated the therapeutic potential of a two-component gel containing ascorbic acid 5% and sodium nitrite 5%; once mixed the gel releases exogeneous NO. Next, Leishmania-resistant C57BL/6 and -susceptible BALB/c mice were infected intradermally with physiological doses of 103 L. major. Mice were treated early on, or – similar to the clinical situation – on fully developed lesions. Treatment was performed 2x/week (200 mg gel). Lesions were significantly smaller in all treatment groups reaching maximal differences starting 2 weeks post treatment (e.g. C57BL/6 4.5±0.8 early treatment groups vs. 10.3±1.2 mm3 in controls, n16). In addition, we observed a significant reduction of the parasite load both after early and delayed treatment as compared to untreated controls (C57BL/6 early: 0.8±0.2 versus 9±2x104 parasites/wk6; late: 1±1 versus 10±3 x104 parasites/wk9, n8). In addition, visceralisation of parasites into spleen was significantly inhibited in all treatment groups. Finally, antigen-specific cytokine release in draining lymph node cells revealed strongly decreased IL-4 and increased amounts of IFNg associated with higher IL-12p40 release in all treatment groups as compared to controls, whereas IL-10 levels remained unaltered. In conclusion, our data indicate that local application of NO donors may be useful in treating newly developed as well as established lesions of L. major infection with no severe side effects. Together with a direct parasite killing effect by exogeneous NO, the mechanism of action is an alteration of the cytokine profile towards Th1-associated protective immunity. 40 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The role of interleukin 22 in Toxoplasma gondii induced ileitis. Melba Muñoz 1, Markus Heimesaat1, Robert Sabat2, Christoph Hoelscher3, Oliver Frey4, Thomas Kamradt4, Wenjun Ouyang5, Oliver Liesenfeld1 1 Institute of Microbiology and Hygiene, Campus Benjamin Franklin, University Hospital Charité Berlin, Germany. 2 Interdisciplinary Group of Molecular Immunopathology, Dermatology/Medical Immunology, Campus Mitte, University Hospital Charité Berlin, Germany. 3Infection immunology, Research Center Borstel, Borstel, Germany, 4Institue of Immunology, Friedrich Schiller University Jena, Germany, 5 Immunology Department, Genentec Inc., South San Francisco, CA USA. Peroral infection in susceptible C57BL/6 mice with Toxoplasma gondii leads to the development of small intestinal inflammation with massive necrosis (pan-ileitis) dependent on Th1 cytokines. The role of Th17 cells in ileitis is unknown. We have previously shown that IL23 but not IL-17 mediates T. gondii-induced small intestinal immunopathology. Therefore, we investigated the role of IL-22 in the development of T. gondii-induced ileitis. IL-23 dependent upregulation of IL-22 was essential for the development of T. gondii-induced small intestinal immunopathology whereas IL-17 was downregulated and dispensable. IL-22-/- mice did not develop small intestinal necrosis although they harbored the same number of parasites as both Wild-type and IL-17-/- mice. Commensal gut flora was also important in the upregulation of IL-22 in the ileum of infected mice. Interestingly, IL-22 was not exclusively produced by CD4+ T cells but also by a non-T non-B cell population in the small intestinal lamina propria. In conclusion, IL-22 induced by IL-23 but not IL-17 is a key mediator of immunopathology in the small intestine. 41 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The role of Frizzled1 in M. tuberculosis infection: Modes of induction and first insights into function Jan Neumann1, Stefan Ehlers2,3, Norbert Reiling1 1 Microbial Interface Biology, 2Microbial Inflammation Research, Research Center Borstel, 23845 Borstel, 3Molecular Inflammation Medicine, Christian-Albrechts University, 24118 Kiel, Germany. Frizzleds represent seven-pass transmembrane receptors for a family of secreted glycoprotein ligands termed "Wnts". Multiple Wnt and Frizzled (Fzd) homologs conduct Wnt/Fzd signaling events through three known pathways: the beta-catenin pathway, the planar cell polarity (PCP) pathway and the Ca2+-dependent pathway. These signaling events assign key functions in embryonic development, stem cell homeostasis and very recently also in inflammation. In the current study we have analysed the regulation of the Wnt/betacatenin pathway in experimental M.tb infection. We observed that the Wnt/beta-catenin signaling is drastically down-regulated in lung homogenates of M.tb-infected mice. In contrast Frizzled1 (Fzd1), a Frizzled homolog associated with beta-catenin signaling, was identified to be up-regulated during M.tb infection. In macrophages Fzd1 mRNA expression is triggered by mycobacteria via TLR2 and MyD88. To gain insights into Fzd1 function in the context of M.tb infection, we analysed the cellular response of macrophages to its ligand Wnt3a, which we find constitutively expressed in lung homogenates of M.tb infected mice. Wnt3a is able to induce beta-catenin signaling in macrophages in a Fzd1-dependent manner. Currently we investigate the functional relevance of Wnt3a and Fzd1 in mycobacteria induced immune responses. 42 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Interaction of Mycobacterium tuberculosis and human macrophages under hypoxic conditions Daniel Nickel1, Steffen Stenger1 1 Institute for Medical Microbiology and Hygiene, University Hospital of Ulm, Germany Mycobacterium tuberculosis (MTb) is an intracellular pathogen that has adapted to the milieu of human lung tissue. Most strikingly mycobacteria manage to survive within a defined cellular conglomerate termed granuloma. Recent studies indicate that oxygen tension in granulomatous areas is far lower as compared to the environmental atmosphere even though exact figures are not available. Due to technical obstacles this physiological situation has not been sufficiently considered in the past when immunological analyses were performed. Therefore we established a model to co-culture human macrophages and virulent MTb under hypoxic conditions. Using a hypoxia chamber integrated in our high safety air flow system we demonstrated that bacterial uptake, cytokine release (IL-10, CCL5, TNF), intracellular growth and cellular viability were virtually identical at 20% O2 and 3% O2. Therefore the interaction of human macrophages and MTb appears to be stable across a broad range of oxygen tension. Western Blotting of macrophages for HIF-1alpha, a surrogate marker of anaerobic metabolism, revealed that this molecule is not yet stabilized at 3%, the condition used in our experiments. However, an oxygen tension of 1% induces anaerobic metabolism, i.e. expression of HIF-1 alpha, without disturbing cellular viability. Ongoing studies are investigating whether further restriction of oxygen availability to 1% or lower will alter the immunological features of the host pathogen interaction in human tuberculosis. 43 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Role of type I IFNs in innate defence to Legionella pneumophila Bastian Opitz Department of Internal Medicine/Infectious Diseases and Pulmonary Medicine, Charité Universitätsmedizin Berlin, Augustenburger Platz 1, 13353 Berlin, Germany Legionella pneumophila, a Gram-negative facultative intracellular bacterium, is the causative agent of a severe pneumonia known as Legionnaires´ disease. Classically, type I IFNs (IFNalpha/beta) have been associated with antiviral immunity. IFN-alpha/beta signal through the IFN-alpha/beta receptor (IFNAR) leading to induction of hundreds of IFN-stimulated genes (ISGs), many of which have anti-microbial activities. Recently, it was demonstrated that type I IFNs are also produced in host cells infected with (intracellular) bacteria or stimulated with cytosolic DNA. These responses were mediated by a so far unidentified cytosolic pattern recognition receptor, and independent of the Toll-like receptors, NOD-like receptors as well as RIG-like receptors. Here we show by RNAi and overexpression assays that L. pneumophila-infected host cells produced IFN-beta dependent on IRF3, but independent of the recently suggested pattern recognition receptor ZBP1 (DLM-1/DAI). We observed enhanced L. pneumophila replication in mouse macrophages lacking IFNAR and human cells after IRF3 knock-down, suggesting that endogenously produced IFN-beta activates a cell-autonomous defence against Legionella. Moreover, IFN-beta treatment restricts Legionella replication in human and murine host cells. Type I IFNs appear not to influence the establishment of the Legionellacontaining vacuole (LCV) or fusion of the LCV with the lysosome. Moreover, type I IFNmediated cell-autonomous defence was independent of autophagy and pyroptosis. We thus hypothesize a crucial involvement of antibacterially acting ISGs. Ongoing studies focus on the role of IFN-induced immunity-related GTPases (IRGs). 44 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Tumor-derived Prostaglandin E2 and TGF-beta synergize to inhibit PDC-derived IFNalpha Isabelle Bekeredjian-Ding1, Meike Schäfer2, Evelyn Hartmann3, Marijo Parcina1, Stefan Endres2, Barbara Wollenberg4, Gunther Hartmann2,3 1 Hygiene-Institute, Dept. of Medical Microbiology and Hygiene, UniversityHospital Heidelberg 2 Dept. of Internal Medicine, Division of Clinical Pharmacology, University of Munich 3 Institute for Clinical Biochemistry and Pharmacology, University Hospital Bonn 4 Department of Otorhinolaryngology, University of Schleswig-Holstein Due to their capacity to produce high levels of type I interferons (IFN-I) plasmacytoid dendritic cells (PDC) are the major targets for adjuvant therapies with CpG ODN. However, PDC infiltrating tumor tissues often lose their IFN-secreting capacity. The tumor environment is characterized by the presence of high concentrations of immunosuppressory mediators such as PGE2, IL-10 and TGF-b. Here we show that prostaglandin E2 (PGE2) and TGF-b increase IL-6 and IL-8 and synergistically inhibit IFN-a and TNF production upon TLR7- or TLR9-mediated activation of human PDC. Receptor expression studies showed that the effects of PGE2 are most likely mediated by EP2 receptor engagement. Further phenotypical characterization of PGE2 and TGFb-treated PDC revealed a down-regulation of CD40 paralleled by an up-regulation of CD86. PDC interaction with other infiltrating immune cells may thus be skewed to a tolerogeneic action at the tumor site. Moreover, PGE2 and TGF-b increase CXCR4 and decrease CCR7 in TLR-stimulated PDC suggesting that PDC lose their ability to migrate to the lymph node and may be retained in the periphery. We therefore speculate that cyclooxygenase inhibitors and TGF-b antagonists may improve TLR7 and TLR9-based immunotherapy in diseases associated with immunosupression. 45 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Systemic bacterial infection alters differentiation of dendritic cells in the bone marrow and mediates chronic dendritic cell dysfunction Eva Pastille1, Yang Zhang2, Nadine Kroell1, F. Ulrich Schade1, Stefanie B. Flohé1, 1 Surgical Research, Department of Trauma Surgery, University Hospital Essen, Essen, Germany; 2Department of Molecular Biology, University Hospital Essen, Essen, Germany Polymicrobial sepsis rapidly causes a dysfunction of dendritic cells (DC) that is maintained even after resolution of the infection. This dysfunction is characterized by an impaired capacity of DC to secrete the Th1-polarizing cytokine IL-12 and to induce a protective Th1 cell response, while the production of IL-10 is enhanced. The long-lasting DC dysfunction causes an enhanced susceptibility to secondary infections that represent life-threatening complications for sepsis patients. We investigated whether DC dysfunction is mediated by a defective differentiation of DC from bone marrow. Sepsis was induced in mice by cecal legation and puncture (CLP) and 4 d after CLP or sham operation, when mice recovered from sepsis, DC differentiation from bone marrow was analyzed in vitro. Upon stimulation with CpG and CD40 ligand, bone marrow-derived dendritic cells (BMDC) from septic mice released extended levels of IL-10 but similar levels of IL-6 compared to sham-BMDC. When injected subcutaneously, BMDC from septic mice showed a reduced capacity to promote Th1-cell polarization. Intranasal application of BMDC from septic mice along with Pseudomonas aeruginosa into naïve mice impaired bacteria clearance in the lung. Lungs of mice treated with BMDC from septic mice contained less IL-12 and IFN-gamma in comparison to lungs of mice injected with sham-BMDC. Co-cultures of BMDC and naive peritoneal macrophages showed an enhanced level of IL-10 upon Pseudomonas aeruginosa stimulation when BMDC derived from septic mice. Thus, during systemic bacterial infection DC follow an altered developmental pathway and mediate chronic immunosuppression through interference of the innate and adaptive immune system. 46 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The phosphatidylserine binding protein annexin A5 can interfere with chlamydial infection Lisa Pfleiderer1, Jan Rupp2, Martin Herrmann3 and Ger van Zandbergen1 1 Institute for Medical Microbiology and Hygiene, University Clinic of Ulm. 2Institute for Medical Microbiology and Hygiene, Center for Structural and Cell Biology in Medicine, University of Lübeck. 3Department for Internal Medicine 3 University Hospital Erlangen Chlamydophila pneumoniae (Cp) is an obligate intracellular pathogen causing respiratory disease. Cp can transfer itself between host cells without being detected by the immune system. It has been suggested that Cp can be released from infected cells hiding in apoptotic bodies. These dying cell parts, present phosphatidylserine (PS) as an apoptotic eat me signal for phagocytes. Recognition of PS induces a non-inflammatory uptake-mechanism and can be blocked by the PS-binding protein annexin-A5 (AnxA5). In this study we focus on chlamydial release of dying infected epithelial cells. In addition we investigated the role of PS on infected apoptotic granulocytes for chlamydial transfer to macrophages. First we used HeLa cells transgenic for GFP on the endoplasmatic reticulum (ER), since it was suggested that apoptotic bodies consist of ER-membrane. Chlamydia infected transgenic HeLa cells were monitored using timelapse imaging. We found that 4 days after infection chlamydia.was present outside the HeLa cells in ER-GFP apoptotic bodies. To study the effect of AnxA5 on chlamydial infection we used 3 day old Cp infected polymorph nuclear neutrophil granulocytes (PMN), one of the first host cells in the lung. We transferred chlamydia from these apoptotic PS-positive cells to either macrophages or alveolar macrophages, as other potential lung host cells. Co-incubation with AnxA5 resulted in a lower infection rate and the presence of smaller Cp. inclusions. Our data suggest that chlamydia can hide in PS-positive apoptotic bodies, in part consisting of ER-membrane. Recognition of PS is an important step in the silent propagation of chlamydia. 47 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Acute graft-versus-host-disease after reduced intensity conditioning is mediated by MyD88 mediated TLR9 sensing of bacterial DNA and can be modulated by administration of TLR9 antagonist Rita Plickert,1 Markus M. Heimesaat,1 Axel Nogai,2 Stefan Bereswill,1 André Fischer,1 Christoph Loddenkemper,3 Ulrich Steinhoff,4 Eckhard Thiel,2 Marina Freudenberg,5 Ulf B. Göbel1 und Lutz Uharek2 1 Institut für Mikrobiologie und Hygiene, Charité - Universitätsmedizin Berlin, Charité Centrum 5, Campus Benjamin Franklin, Hindenburgdamm 27, D-12203 Berlin, Germany 2 Medizinische Klinik III (Hämatologie, Onkologie und Transfusionsmedizin), Charité - Universitätsmedizin Berlin, Charité Centrum 14, Campus Benjamin Franklin, Hindenburgdamm 30, D-12200 Berlin, Germany 3 Institut für Pathologie, Charité - Universitätsmedizin Berlin, Campus Benjamin Franklin, Hindenburgdamm 30, D-12200 Berlin, Germany 4 Max Planck Institute of Infection Biology, Schumannstrasse 20-21, 10117 Berlin, Germany 5 Max Planck Institut für Immunbiologie, Stübeweg 51, D-79108 Freiburg, Germany Graft-versus-host-disease (GvHD) is a major cause for morbidity and mortality after allogeneic stem cell transplantation. Acute intestinal GvHD is mediated by bacterial sensing via toll-like-receptors (TLR), but the immunobiology in situ is poorly understood. In a murine stem cell transplantation model based on reduced intensity conditioning, we investigated the impact of bacterial sensing via TLRs on intestinal GvHD. Following transplantation, wild type mice displayed intestinal tissue damage, accompanied by elevated numbers of T-cells, neutrophils, apoptotic and proliferating cells in the colon. In TLR9-/- mice the numbers of Tcells, neutrophils and apoptotic cells after transplantation in the colon were significantly reduced, resulting in amelioration of the tissue damage and in improved survival of TLR9 deficient mice. Similar changes were observed in MyD88-/- mice, supporting our results in TLR9-/- mice. The administration of a TLR9 antagonist in wild type mice after transplantation showed similar results as demonstrated in TLR9-/- and MyD88-/- mice, indicating that intestinal GvHD can be influenced by the modulation of TLR9 sensing. These results indicate an important role of TLR9 in the pathomechanism of GvHD and may lead to a therapeutic approach in the future. 48 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Split tolerance after oral vaccination of mice with recombinant Escherichia coli Nissle 1917 expressing fimbrial adhesin K88 Katharina A. Remer, Marita Bartrow, Bianca Roeger, Heidrun Moll, Tobias A. Oelschlaeger University of Würzburg, Institute for Molecular Infection Biology, Würzburg, Germany Probiotic bacteria are live, non-pathogenic micro-organisms which are beneficial for the health of the host. One of these, the Escherichia coli strain Nissle 1917 (EcN) is used as a probiotic agent for the treatment of infectious and chronic inflammatory diseases of the intestine. Since it has been shown that EcN can serve as a safe carrier for targeted delivery of recombinant molecules to the intestinal mucosa, we constructed the recombinant strain EcN pMut2-kanK88 (EcN-K88) stably expressing the determinant for the K88 fimbrial adhesin on the bacterial surface. K88 is a key virulence factor of enterotoxigenic E. coli (ETEC), which are the cause of one of the economically most important diseases in swine husbandry. Massive efforts have therefore been made to develop a vaccine for the induction of protective mucosal immunity against ETEC. After oral application of EcN-K88 to mice for one week, EcN-K88 as well as wild-type EcN and EcN mock-transformed with the plasmid vector only could be detected in faecal samples for a prolonged period of time after the last feeding, indicating that EcN can transiently colonise the murine intestine. Oral application of EcN-K88 resulted in significant IgG serum titers against K88 as early as seven days after the initial feeding with EcN-K88, but no significant IgA titers. In contrast, we failed to detect any specific T cell responses towards the K88 antigen both in spleen and mesentheric lymph nodes. Although dendritic cells readily up-regulated maturation and activation markers in response to K88 stimulation, accompanied by secretion of interleukin (IL)-12, IL-6, IL-10 and tumour necrosis factor, restimulation of T cells from mice having received EcN-K88 with K88-loaded dendritic cells did not result in detectable T cell proliferation and IL-2 secretion, but rather induced an IL-10 bias. While the serum antibody responses clearly demonstrate that K88 is recognized by the humoral immune system, our findings indicate that oral application of probiotic EcN expressing the K88 fimbrial adhesin induces a selective T cell tolerance towards the antigen. 49 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Wnt ligands differentially regulate the inflammatory response of macrophages upon mycobacterial infection Kolja Schaale1, Stefan Ehlers2,3 and Norbert Reiling1 1 Microbial Interface Biology, 2Microbial Inflammation Research, Research Center Borstel, 23845 Borstel, 3Molecular Inflammation Medicine, Christian-Albrechts University, 24118 Kiel, Germany. Wnt proteins are secreted palmitoylated glycoproteins with multiple functions in cell proliferation, migration as well as tissue organization. They are best known for their role in embryonic development and tissue homeostasis. Deregulation of Wnt signaling has been shown to promote carcinogenesis. Recently we identified Wnt signaling to be involved in the regulation of inflammatory processes: Wnt5a is induced in human macrophages in response to mycobacteria and conserved bacterial structures and contributes to the regulation of the proinflammatory cytokines IL-12 and IFN-gamma. To gain deeper insights into Wnt mediated modulation of inflammatory processes we now used murine bone marrow derived macrophages and analyzed the effects of the addition of exogenous Wnt homologs. We monitored Wnt-mediated activation of primary macrophages by measuring the activation of signaling pathways and transcription factors, analyzed the expression of target genes by Real-Time PCR and measured the secretion of inflammatory cytokines by ELISA. Exogenous Wnt5a - but not Wnt3a - was able to induce cytokine expression in primary macrophages. In infection experiments Wnt5a promoted the mycobacteria-induced macrophage activation and enhanced the expression of inflammatory mediators in murine macrophages. In contrast, addition of Wnt3a reduced the expression of inflammatory mediators upon mycobacterial infection. These data corroborate our previous findings and further support the notion that TLR/NF-kappaB and Wnt signaling, both being evolutionary highly conserved pathways, are functionally interconnected. 50 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Induction of pro-inflammatory IL-12 in Plasmodium berghei infected BALB/c mice breaks blood-brain-barrier and leads to cerebral malaria Kim Ellen Schmidt1, Beatrix Schumak2, Sabine Specht1, Bettina Dubben1, Frank Juengerkes2, Volker Schmitz3, Andreas Limmer2 and Achim Hoerauf1 1 Institute of Medical Microbiology, Immunology and Parasitology, University Hospital Bonn 2 Institute of Molecular Medicine and Experimental Immunology, University Hospital Bonn 3 Department of Internal Medicine I, University Hospital Bonn, Infection with Plasmodium parasites causes malaria and often results in development of severe complications like severe malaria anaemia or cerebral malaria, which are mainly attributed to overwhelming inflammatory immune reactions of the host. Murine models that differ in the development of experimental cerebral malaria (ECM) allow detailed studies of host responses towards infection with the rodent malaria parasite Plasmodium berghei ANKA (PbA). Here we show that BALB/c mice, which are known to be resistant against experimental cerebral malaria can be driven into interferon-gamma (IFN-gamma) dependent ECM pathology and subsequent death if they received CpG after Plasmodium infection. CpG application resulted in production of pro-inflammatory cytokines as well as neuro-pathological symptoms, like hemiplegia, convulsions, coma leading to increased mortality. Importantly, CpG application caused permeabilization of the blood brain barrier, comparable to ECMsusceptible PbA infected C57 BL/6 mice. Experiments in genetically deficient mice revealed that ECM development in BALB/c mice after CpG application was dependent on the presence of interleukin 12. The pathological consequences of CpG application could be ascribed to interleukin 12 as similar results were obtained with injection of recombinant Adenovirus expressing interleukin 12. Taken together our data suggest that the induction of pro-inflammatory mediators provokes ECM development in BALB/c mice in an IL-12 dependent manner. 51 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Airway epithelial cells modify immune responses Lotte M. Schmidt, Magdalena Dahmen, Fabian Fey and Alexander H. Dalpke Department of Hygiene and Medical Microbiology, University of Heidelberg, Germany Airway epithelial cells are lining the body’s largest surface and represent the first line of defence against invading pathogens. Moreover, they are also playing an important role in innate mucosal immunity by secretion of antibacterial proteins. Nowadays, it turns out that the airway epithelium also has simple immune functions, mediated in part by the expression of TLRs. However, as upper airways are not an entirely sterile compartment the question was raised how local immunity and homeostasis is regulated. We speculated that epithelial cells within the airway microenvironment are regulators of professional immune cells. We show that epithelial-cell conditioned dendritic cells display properties of alternative activation with increased expression of arginase-1 and interleukin 10 and reduced TLR-mediated upregulation of CD40, CD86 and pro-inflammatory cytokines. These “alternative “activated dendritic cells also showed a reduced capacity of induction of T-cell proliferation. Modulation of T-cell proliferation by epithelial cells was mediated in two different ways, first directly via TGF-beta and second indirectly via the influence on antigen presenting cells. Modified T cells showed increased differentiation towards interleukin 10 producing Tr1 cells. Our results indicate that bronchial epithelial cells are capable of inducing a non-inflammatory microenvironment. Furthermore we now hypothesize that during infections this inhibition is transiently down-regulated resulting in a “release of inhibition”. First results with supernatant showed that the infection of epithelial cells in the absence of further immune cells is not sufficient to convert this anti-inflammatory microenvironment into an immune activated state. This hints towards a role of migratory immune cells invading the lung during infection. 52 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Influence of optineurin on adenovirus E3-14.7K mediated TNF-resistance Laura Klingseisen; G.Knoll; M.Kurz; Wulf Schneider-Brachert Institute for Med. Microbiology; University of Regensburg Recently we have shown, that adenovirus E3-14.7K (14.7K) expressing cells are protected from TNF-mediated apoptosis by inhibition of TNF-Receptor-1 (TNFR1) internalization. In the presence of 14.7K the recruitment of essential adaptorproteins involved in both apoptosis signalling (TRADD, FADD, and caspase-8) and clathrin-mediated endocytosis (rab5 and dynamin2) to the activated TNFR1 is blocked. The 14.7K interacting protein optineurin seems to link 14.7K not only to the apoptotic pathway but also to the membrane trafficking network via its additional interacting partners rab8 and huntingtin. Therefore we investigated wether the interaction of 14.7K with optineurin is essential to prevent TNF-mediated apoptosis. We generated several mutants of 14.7K and characterized their ability to protect cells from apoptosis and to interact with optineurin. Finally 14.7K expressing cells were treated with optineurin targeting siRNA to examine the importance of optineurin for 14.7K mediated inhibition of apoptosis. The 14.7K mutants defined three groups: (i) ones, which interacted with optineurin and protect cells from cell death, (ii) others that interacted with optineurin but failed to protect, and those (iii) that were incapable for interaction and inhibition of apoptosis. Interestingly the suppression of optineurin by siRNA transfection did not revert the TNF-resistant phenotype. Collectively, these data suggest that optineurin might not be essentially involved in 14.7K mediated inhibition of TNFR1 induced apoptosis. Additional work is under progress to address the effect of optineurin on TNFR1internalization. 53 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Activation of macrophages by the mycobacterial cord factor (TDM) and its synthetic analogue (TDB) Hanne Schoenen7, Kerstin Werninghaus1,7, Anna Babiak1, Olaf Groß2, Christoph Hoelscher3, Else Marie Agger4, Falk Nimmerjahn6, Juergen Ruland2, and Roland Lang1,7 1 Institute of Medical Microbiology, Immunology and Hygiene, Technical University Munich, D- 81675 Munich, Germany; 2Department of Hematology, Technical University Munich, 80333 Munich, Germany; 3Division of Infection Immunology, Research Center Borstel, D-23845 Borstel, Germany; 4 Adjuvant Research, Department of Infectious Disease Immunology, Statens Serum Institute, 2300 Copenhagen, Denmark; 5Semmelweis University School of Medicine, Budapest H-1089, Hungary; 6 Molecular Medicine, 7 Institute Microbiology, University Hospital Erlangen, 91054 Erlangen, Germany; of 8 Clinical Division of Immunology, CLS, Institute for Infectious Diseases and Molecular Medicine, University of Cape Town, 7925 Cape Town, South Africa Mycobacterium tuberculosis (MTB) causes nearly two million deaths per year. The live vaccine M. bovis (BCG) does not prevent pulmonary tuberculosis and can not be used in immunocompromised people. Immunization with recombinant subunit vaccines is an attractive new vaccination strategy. These subunit vaccines require adjuvants that trigger innate immunity which then activate the adaptive immune system. In mouse vaccination studies the mycobacterial cord factor Trehalose-6, 6-dimycolate (TDM) and its synthetic analogue Trehalose-6,6-dibehenate (TDB) have shown to be efficient adjuvants. Injection of the recombinant protein H1 derived from MTB in combination with TDB as adjuvant lead to a strong Th1 and Th17 T-cell response in mice. Furthermore, macrophages and DCs respond with cytokine and NO production in vitro. We have addressed the mechanism of APC activation by TDB and TDM utilizing different techniques. Using knock-out mice it was shown that the response to the glycolipids was independent on the Toll-like receptor associated signalling molecule MyD88 in vitro. Microarray analysis revealed that the stimulation of macrophages with TDB leads to upregulation of several C-type lectins including Dectin-1. However the recognition of these glycolipids was independent of Dectin-1 and Dap12, whereas the adaptor protein Fc-receptor gamma chain was essential. Furthermore, knockout and inhibition studies showed that the Syk-Card9-Bcl10-Malt1 pathway was required for glycolipid recognition. To get more detailed information about the mechanism of APC activation mediated by TDB further investigations are required and will be focused on potential receptor candidates of the C-type lectin family and the signalling events after glycolipid recognition. 54 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 A crucial role of the spleen in the induction of pathogenic host responses towards P. berghei ANKA infection Beatrix Schumak1, Kim Schmidt2, Sabine Specht2, Frank Juengerkes1, Günter J. Hämmerling3, Achim Hoerauf2, Andreas Limmer1 1 Institute of molecular Medicine and experimental Immunology, University Hospital Bonn; 2 Institute of medical Microbiology, Immunology and Parasitology, University Hospital Bonn; 3 German Cancer Research Center, Department of Tumor Immunology, Heidelberg Cerebral malaria is a severe complication of Plasmodium infection and is generally assumed to be an immune-mediated pathology as a result of excessive inflammation. Interferon gamma and activated T cells are among the few factors that are known to be essential for the development of experimental CM (ECM) in susceptible mouse strains upon infection with P. berghei ANKA. It has been long speculated where pathogenic T cells and inflammatory cytokines causing ECM are generated. Among direct effects on the brain, the spleen has been taken into consideration. We show that splenectomized animals were protected against ECM; in addition, our data demonstrate the relevance of an intact micro-architecture of the spleen. PbA infected RAG-deficient mice developed ECM only if they received effector cells from PbA infected wildtype donors but not after transfer of lymphocytes from naïve donors. Furthermore, we determined a crucial role for dendritic cells in the detection of Plasmodium parasites and subsequent induction of detrimental parasite specific immune responses. Mice depleted of DCs or deficient in IL-12p35 were protected against ECM and lacked PbA specific T cells, which emphasizes the importance of these antigen presenting cells in the induction of parasite-specific T cells responses. In addition, support of T cell priming and induction of interferon gamma belong to the most prominent biological functions of IL-12, a cytokine which is almost exclusively produced by DCs. Taken together, our data show the importance of the spleen in the induction of pathological host responses towards blood stage PbA infection in susceptible mice. 55 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Long-term effect of sepsis - The influence of bacteremia and bacterial translocation on systemic adaptive immune responses Timo Schwandt1, Frank Juengerkes 1, Beatrix Schumak1, Gerrit Gielen*, Joerg Kalff2, Percy Knolle1, Bernhard Holzmann3, Andreas Limmer1 1 Institute of Molecular Medicine and Experimental Immunology, University of Bonn, Germany; 2Department of Surgery, University of Bonn, Germany; 3Department of Surgery, Technical University Munich, Germany Bacterial translocation is a possible risk of abdominal surgery and could be the cause of lifethreatening consequences such as organ failure and septic shock. Patients surviving septic shock often suffer from opportunistic infections as well as defects in adaptive immunity. Here, we mimicked abdominal surgery by intestinal manipulation (IM) in mice. To study septic conditions, mice received E.coli expressing luciferase either intravenously or per os prior to subjection to CASP as well as IM. Translocation of gut-derived bacteria was monitored by in vivo imaging (Xenogen) and additional microbiological assays. We detected comparable amounts of bacteria in lung, liver and spleen of mice that underwent CASP or were injected i.v. with E.coli. In contrast, bacteria were detected in lung and liver but not in spleen of mice that were subjected to IM or received E.coli by injection into the hepatic portal vein. Depletion experiments imply that Kupffer cells as well as soluble mediators such as Tumor necrosis factor play an important role in trapping and clearance of translocated bacteria in liver and lung. Our experiments demonstrated that translocation of bacteria did not cause immune suppression as long as they did not reach the spleen in high numbers. We suggest that liver and lung fulfill a filter function to prevent systemic distribution of gut-derived bacteria. Failure of or bypassing these barriers might enable bacteria to access the spleen and thus cause systemic suppression of adaptive immunity. 56 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Functional analysis of cells from IFIT-2 knockout mice Alexandra Siegfried, Susanne Berchtold, Birgit Manncke, Ingo B. Autenrieth, Erwin Bohn Institut für Medizinische Mikrobiologie und Hygiene, UKT Tuebingen Interferon-induced tetratricopeptide repeat protein (IFIT)-2 is a type I interferon induced gene which we found to be highly expressed during Y. enterocolitica infection as well as in a mouse model for IBD. The biological functions of IFIT-2 are so far elusive. It is only known that IFIT-2 may interact with the translation initiation factor eIF3c and may affect protein translation. In addition, hIFIT-2 may interact with cytokeratin and may influence tumor cell migration. In this study IFIT-2 knockout mice were generated to further assess the biological roles of IFIT-2. The effects of mouse IFIT-2 on cell composition, T cell proliferation, B cell maturation, LPS induced cytokine secretion and first results on its regulatory properties will be discussed. 57 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Blockade of IL-6 trans-signalling does not reactivate experimental tuberculosis Jan Christian Sodenkamp,1 Georg H. Waetzig,2 Juergen Scheller,3 Dirk Seegert,2 Stefan Rose-John,3 Stefan Ehlers,4,5 Christoph Hoelscher1 1 Division of Infection Immunology, Research Center Borstel, Borstel, Germany; 2CONARIS Research Institute AG, Kiel, Germany; 3Department of Biochemistry, Christian-AlbrechtsUniversity, Kiel, Germany; 4 Molecular Inflammation Medicine, Research Center Borstel, Borstel, Germany; 5Molecular Inflammation Medicine, Christian-Albrechts-University, Kiel, Germany Therapeutic approaches for chronic inflammatory conditions, such as rheumatoid arthritis and Crohn's disease, using e.g. TNF targeted biologics are associated with an increased risk of infectious complications, especially tuberculosis (TB). The pro-inflammatory cytokine interleukin (IL)-6 can bind to gp130 on cells lacking the IL-6 receptor (IL-6R) when it forms a complex with the soluble IL-6R (sIL-6R) (IL-6 trans-signalling). Trans-signalling is counteracted by soluble gp130 (sgp130). In mice, specific neutralization of the IL-6/sIL-6R complex in vivo by sgp130Fc fusion proteins with 10- to 100-fold higher inhibitory activity than natural sgp130 has been shown to suppress inflammatory bowel disease and ameliorate rheumatoid arthritis. Hence, blockade of IL-6 trans-signalling by sgp130Fc provides a novel approach for the treatment of a range of chronic inflammatory diseases. However, the effect of sIL-6R neutralization on the outcome of experimental TB has not been investigated so far. To evaluate the potential risk of interfering with IL-6 trans-signalling, we analyzed the outcome of experimental TB under treatment with an optimized sgp130Fc fusion protein. C57BL/6 mice were infected with Mycobacterium tuberculosis via the aerosol route. At the onset of experimental TB or during an already established infection, mice were treated with an anti-TNF antibody and with various doses of sgp130Fc for five weeks. Whereas neutralization of TNF resulted in a strikingly impaired cell-mediated immune response followed by pulmonary granuloma desintegration and exacerbated bacterial loads, protective immune responses were unaffected after treatment with sgp130Fc. Our finding that blockade of IL-6 trans-signalling does not reactivate experimental TB implies the treatment of chronic inflammatory diseases with sgp130Fc as a superior approach to avoid adverse consequences of anti-inflammatory strategies. (Supported by the Inflammation Research Excellence Cluster) 58 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Delayed type hypersensitivity versus humoral immune response – Influence of high and low antigen doses on the cytokine expression within splenic compartments Claudia Stamm, Juergen Westermann, Kathrin Kalies Institute of Anatomy, University of Luebeck Immunisations with different antigen doses provoke different immune responses. Thus, injection of a low dose of sheep red blood cells (SRBC) (1x105) induces a delayed type hypersensitivity (DTH) reaction after reexposure to the antigen, whereas the injection of a high dose (1x109) induces a humoral immune response and suppresses a DTH. In order to examine these mechanisms, we investigate the sequence of events occurring in the compartments of the spleen from 1 h after immunisation up to 10 days. After primary injection of a low dose, SRBC are hardly detectable in the spleen. Moreover, the isolation of individual splenic compartments followed by an exponential amplification during real-time RT-PCR is not sensitive enough to detect any changes in cytokine expression before T-cell proliferation takes place after 2-3 days. Interestingly, IFN-gamma expressing cells appear in the B-cell follicles between 3-6 days after immunisation. In contrast after primary injection of a high dose, SRBC localize in the marginal zone and in the red pulp. Increased IL12p40 transcription is found in the marginal zone 4 h after injection and is followed by an increase of IL12p40 and IL2 in the T-cell zone. Surprisingly, compared to the low-dose injection a twofold higher T-cell proliferation is observed after 2-3 days. Overall, Th1-cytokines are usually associated with DTH. As the high-dose immunisation doesn’t induce DTH but unexpectedly upregulates Th1-inducing cytokines, we hypothesize that antigen-specific Th1 cells are induced but unable to reach the skin. 59 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 The role of the intestinal microflora in infection with Citrobacter rodentium Stephen T. Reece, Anne Kohler, Petra Krienke, Marcus Heimessat, Ulrich Steinhoff Max-Planck Institute für Infektionsbiologie and Charité Universitätsmedizin, Institut für Mikrobiologie und Hygiene, Berlin Citrobacter rodentium (C. rodentium) is a gram negative enteric pathogen that triggers intestinal inflammation and hyperplasia. During infection, the bacillus attaches to the colonic epithelium and forms attaching and effacing (A/E) lesions, analogous to the groups of human gastrointestinal pathogens Enterohaemorraghic Escherichia coli (EHEC) and Enteropathogenic E. coli (EPEC). After infection via the oral route, the bacterium rapidly colonises the host colonic epithelium, induces an acute colonic inflammatory response that peaks between day 7 and 14 post infection and susceptible mouse strains and certain genetic KO mice succumb at this timepoint. Resistant mouse strains rapidly clear C. rodentium from the colon with very low or absent bacterial titres present by day 28 post infection. It has been postulated that C. rodentium utilises A/E lesion formation to out compete normal flora to attach to the colonic epithelium and A/E lesion formation is critical for both colonisation of the host and the local inflammatory response. However, the role of normal colonic microflora during C. rodentium infection has not yet been addressed. In the present study we show that despite being a carrier of C. rodentium, infection is not lethal for germfree mice. Interestingly, the association of normal flora to previously germfree mice that have been infected C. rodentium mice will lead to bacterial clearance in these animals. Our data indicate that bacterial resistance is not due to antibodies but to the regulation of genes of the fat-metabolism which are induced by the intestinal microflora. 60 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 IL-4/IL-13-dependent alternative activation of macrophages but not microglial cells is associated with uncontrolled cerebral cryptococcosis Werner Stenzel1, Uwe Müller2,4, Gabriele Köhler3, Frank L. Heppner1, Manfred Blessing2,4, Andrew N.J. McKenzie5, Frank Brombacher6, and Gottfried Alber2 1 Department of Neuropathology, Charité Universitätsmedizin, Berlin, Germany; 2Institute of Immunology, College of Veterinary Medicine, University of Leipzig, Leipzig, Germany; 3 Gerhard Domagk Institute for Pathology, University of Münster, Münster, Germany; 4 Molecular Pathogenesis, College of Veterinary Medicine, Center for Biotechnology and Biomedicine, University of Leipzig, Leipzig, Germany; 5Medical Research Council Laboratory of Molecular Biology, Cambridge, United Kingdom; 6Institute of Infectious Disease and Molecular Medicine and International Centre for Genetic Engineering and Biotechnology, University of Cape Town, Cape Town, South Africa IL-4- and IL-13-dependent Th2-mediated immune mechanisms exacerbate murine Cryptococcus neoformans-induced bronchopulmonary disease. To study the roles of IL-4 and IL-13 in cerebral cryptococcosis, interleukin (IL)-4 receptor a-deficient (IL-4Ra-/-), IL-4deficient (IL-4-/-), IL-13-deficient (IL-13-/-), IL-13 transgenic (IL-13T/+), and wild-type (WT) mice were infected intranasally. IL-13T/+ mice displayed higher fungal brain burden than WT mice, whereas the brain burden of IL-4Ra-/-, IL-4-/-, and IL-13-/- mice was significantly lower as compared to WT mice. Upon infection 68 % of WT mice, and 88 % of IL-13-overexpressing IL-13T/+ mice developed cerebral lesions. In contrast, IL-4Ra-/-, IL-4-/-, and IL-13-/- were essentially protected from CNS invasion by the fungus. Furthermore, IL-13T/+ mice harbored large pseudocystic lesions in the CNS parenchyma, bordered by voluminous foamy alternatively activated macrophages (aaMph) containing intracellular cryptococci. In WT mice, also aaMph tightly bordered pseudocystic lesions. In resistant IL-4-/-, IL-13-/-, and IL4Ra-/- mice, no aaMph were discernible. Microglial cells of all mouse genotypes neither internalized cryptococci nor were found to express markers of alternative activation although they displayed similar IL-4Ra expression as macrophages. These data provide first evidence of the development of aaMph in a CNS infectious disease model and point to distinct roles of macrophages vs. microglial cells in the CNS immune response against C. neoformans. 61 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Identification of a novel subcellular localization pattern of Suppressor of Cytokine Signaling-1 (SOCS-1) Julia Strebovsky, Andrea Baetz, Christian Koelsche, Alexander H. Dalpke Dept. of Hygiene and Medical Microbiology, University Heidelberg Suppressor of cytokine signaling (SOCS) proteins are inducible feedback inhibitors of janus kinases and signal transducer and activator of transcription (STAT) signaling pathways. SOCS proteins are induced by various cytokines as well as Toll-like receptor (TLR) ligands and are supposed to act inhibitory at the level of cytokine receptor phosphorylation, janus kinase activation or STAT recruitment. We surprisingly observed that SOCS-1, but no other members of the SOCS family, predominantly localizes to the nucleus which could be attributed to a novel bipartite nuclear localization signal (NLS) located between the SH2 domain and the SOCS box. Using a mutational approach the NLS could be narrowed down to several pivotal arginine amino acids. Although primarily expressed within the nucleus a fraction of GFP-SOCS-1 was also observed within the cytoplasm being ligated to the plasma membrane. GFP-SOCS-1 was demonstrated to clearly suppress IFN-alpha mediated STAT1 phosphorylation. GFP-SOCS-1 proteins bearing mutations in the NLS evidently showed a loss of nuclear localization and were still able to interfere with STAT activation, however were less inhibitory in STATdependent reporter assays. To further analyse the role of nuclear SOCS-1 inducible cell-lines have been established. Using photoactivable SOCS-1 constructs we could confirm that translocation from the cytoplasm to the nucleus occurs very rapidly and that SOCS-1 is highly mobile within the nucleus. Thus, we claim a new role for SOCS-1 which is independent from feedback inhibition of Jak/STAT pathways but dependent on its nuclear availability. 62 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Improvement of host defense in the lung Thomas Tschernig, Felicitas Hecke, Tanja Kerber-Momot, Ulrich Maus, Reinhard Pabst. Medizinische Hochschule Hannover, Carl-Neuberg-Str. 1, 30625 Hannover MALP-2 is a synthetic lipopeptide and a specific ligand of TLR-2/6. It stimulates the host defense by induction of chemokines and proinflammatory cytokines. In cocultures with rat alveolar macrophages and M. bovis BCG MALP-2 led to an enhanced killing of the bacilli. After intratracheal infection of mice with M. bovis BCG and simultaneous MALP-2 application decreased numbers of the bacteria were found in the BAL and the lung homogenate at different times of analyses. In an acute model of lung infection caused by P. aeruginosa MALP-2 lead to reduced numbers of bacteria in the lung tissue and to a better clinical course of the infection when the application was performed one day prior to the infection. Thus, local stimulation of the pulmonary immune system via the TLR-2/6 improves host defense to bacteria in the lung. 63 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Detrimental role of dendritic cells during Y. enterocolitica infection in vivo Philipp Warnke1, Tanja Linzer2, Sandra Schmitz1, Ingo B. Autenrieth1, Stella Autenrieth1,2 1 Institute of Medical Microbiology and Hygiene, University Hospital of Tübingen, Tübingen, Germany; 2Department of Immunology, University of Tübingen, Tübingen, Germany CD4 T cells have been demonstrated to be required for control of Yersinia enterocolitica infection in mice. However, virulence factors of Y. enterocolitica may inhibit T cell priming by targeting dendritic cells (DC) in several ways: inhibition of maturation and antigen uptake as well as by the induction of cell death as demonstrated in bone marrow-derived DC. Here we investigated the role of DC in severe Y. enterocolitica infection in vivo using C57BL/6 wild type and transgenic mice expressing the diphtheria toxin (DT) receptor under the control of the CD11c promoter (CD11c.DOG mice) in order to deplete DC in vivo. Repetitive application of DT led to significant ablation of DC. Upon Y. enterocolitica infection of wild type and DC depleted CD11c.DOG mice we observed less bacterial burden in the spleen one to 7 days post infection in CD11c.DOG mice compared to wild type mice and a better survival of the CD11c.DOG mice compared to the wild type mice. We also observed less viable intracellular Y. enterocolitica in CD11b+ and Gr-1+ cells one day post infection in CD11c.DOG mice compared to wild type mice. No difference in the cell populations in the spleen could be observed one day post infection between the two mouse strains. However, the number of CD11b+ and Gr-1+ cells was increased in the spleen of CD11c.DOG mice compared to wild type mice at later time points. One day post infection CCL2, CCL4, CCL7, and IFN-gamma mRNA expression was increased 12 to 35 fold in wild type mice compared to CD11c.DOG mice. Adoptive transfer of CFSE-labeled OVA-specific CD4+ T cells into CD11c.DOG mice treated with DT and infected with Y. enterocolitica revealed reduced proliferation rates compared to control mice. Taken together, our data suggest that DC may play an ambiguous role in Y. enterocolitica infection: DC contribute to increased cytokine and chemokine production and T cell priming, but upon high dose Y. enterocolitica infection may contribute to increased bacterial burden and mortality. 64 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Injury-induced Th cell suppression after injury is restored through targeting dendritic cells in the regenerating tissue Florian Wirsdörfer, Jörg Martin Bangen, Michaela Bak, F. U. Schade, Stefanie Flohé Surgical Research, Department of Trauma Surgery, University Hospital Essen, Virchowstr.171, D-45147 Essen Severe injury causes a broad deterioration of the immune system that leads to an enhanced susceptibility to infectious complications. In parallel, repair/regeneration processes are initiated in order to restore tissue integrity. We investigated whether dendritic cells (DC) that appear in the regenerating tissue after skeletal muscle injury might modulate the immune response to a microbial antigen. A blunt soft tissue trauma of the gastrocnemius muscles of mice was induced through a single drop-mass impact. One, 4, or 7 d later, leukocyte infiltration in the muscles and specific T cell responses to ovalbumin/LPS as model antigen in the popliteal lymph nodes (LN) were characterized. DC in the damaged tissue increased in number from day 4 after trauma and continuously increased the expression of MHC class II, CD40, and CD86. After intramuscular application of FITC-labelled ovalbumin, the percentage of ovalbumin-FITC positive DC was higher in draining LN from trauma than from sham mice indicating migration of DC from the muscle into the LN. Ovalbumin-specific Th-cells in the LN of trauma mice secreted higher levels of IFN-gamma than cells from sham mice when ovalbumin/LPS was applied into the gastrocnemius muscle on day 7 but not earlier after injury. The proliferation of antigen-specific T cells remained unaffected. In contrast, upon application of ovalbumin/LPS distant to the site of injury, namely into the footpad, the ovalbumin-specific IFN-gamma secretion in the popliteal LN was suppressed. Thus, Th cell responses are impaired after skeletal muscle injury but can be restored through targeting DC in the regenerating tissue. 65 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 TLR agonist R848 inhibits differentiation of mDCs and leads to differentiation of tolerogenic APC from CD14+ monocytes Sabine Woelfle1, Aline Gierschke1, Klaus Heeg1 1 Dept. of Hygiene and Medical Microbiology, University of Heidelberg, Germany We have shown previously that TLR agonists interfere with GMCSF and IL4 (G4) driven differentiation of immature mDC from CD14+ monocytes in vitro. Among the TLR agonists the TLR7/8 agonist R848 is the strongest inhibitor of mDC differentiation. Stimulation of CD14+ monocytes with G4 and R848 resulted within 5 days in a cell type that is characterized by an increased PDL-1 and a decreased CD1a expression. The induced deviant APCs preferentially induce CD25+ FoxP3+ T regulatory cells. We have started to analyse the mechanisms of action. Therefore we determined cytokine secretion and MAPkinases activation: In comparison to G4 stimulated monocytes, R848 plus G4 stimulated monocytes released high IL-6 amounts and TNF, IL-10 and IL-12p40. Because of the ability of IL-6 to prevent upregulation of CD1a we blocked the IL-6 signalling pathway and investigated STAT-3 phosphorylation. IL-6 alone was not responsible for the decreased CD1a expression. However STAT-3 phosphorylation was enhanced by R848 plus G4. There were also differences in the MAPK activation pattern. Upon stimulation with R848 and G4 a strong JNK phosphorylation was observed which was not seen with G4 alone. P38 was also stronger phosphorylated in R848 plus G4 stimulated cells. P44/42 phosphorylation was higher with R848 and G4 within the first 15 min. However, at later time points p44/42 phosphorylation was lower. Inhibition of p44/42 lead to downregulation of PD-L1 as STAT-3 inhibition did. We suggest a link between p44/42 and STAT-3 phosphorylation. Here we present first hints, that this could be indeed the case. 66 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 LIST OF PARTICIPANTS Name Institute Email 1. Alber, Gottfried Universität Leipzig, Veterinärmedizinische Fakultät, Immunologie [email protected] 2. Bang, Claudia Universität Lübeck, Institut für Anatomie [email protected] 3. Bank, Elena Universitätsklinikum Hygiene 4. Bart, Thomas Universität Regensburg, Institut für Immunologie [email protected] 5. Barthelmann, Julia Universität Lübeck; Institut für Anatomie [email protected] [email protected] Ulm; Medizinische Mikrobiologie und [email protected] 6. Bauer, Judith 7. Behrends, Jochen Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Forschungszentrum Borstel; Infektionsimmunologie 8. Bekeredjian-Ding, Isabelle Universität Heidelberg; Medizinische Mikrobiologie [email protected] 9. Bogdan, Christian Universität Erlangen; Medizinische Mikrobiologie [email protected] 10. Bohn, Erwin Borkens, Stephanie Universität Tübingen, Institut für Medizinische Mikrobiologie und Hygiene Universität Düsseldorf; Medizinische Mikrobiologie [email protected] 11. 12. Bruder, Dunja Helmholtz-Zentrum für Infektionsforschung, Braunschweig [email protected] 13. Chittappen Kandiyil, Prajeeth Dalpke, Alexander 15. Degrandi, Daniel Universität Erlangen, Institut für Klinische Mikrobiologie, Immunologie und Hygiene Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Universität Düsseldorf; Medizinische Mikrobiologie [email protected] 14. 16. Deininger, Susanne [email protected] 17. Didovic, Sonja Universitätsklinikum Bonn, Institut für Medizinische Mikrobiologie, Immunologie und Parasitologie Universität Düsseldorf, Düsseldorf Institut für umweltmedizinische Foschung 18. Dietze, Kirsten Universitätsklinikum Essen, Institut für Virologie [email protected] 19. Dresing, Phillip Universität Düsseldorf; Medizinische Mikrobiologie [email protected] [email protected] [email protected] [email protected] [email protected] [email protected] Sonja. [email protected] 20. Durlanik, Sibel 21. Eberle, Florian Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Universität Heidelberg; Medizinische Mikrobiologie 22. Echtennacher, Bernd Universität Regensburg; Immunologie [email protected] 23. Ehlers, Stefan Forschungszentrum Borstel, Molekulare Entzündungsmedizin [email protected] 24. Enzenmüller, Stefanie Universitätsklinikum Hygiene 25. Erdmann, Hanna Forschungszentrum Borstel, Infektionsimmunologie [email protected] 26. Fischer, Anna Universität Düsseldorf, Institut für medizinische Mikrobiologie [email protected] 27. Fischer, Michael Universität Mainz, Institut für Dermatologie [email protected] 28. Flohe, Stefanie Universitätsklinikum Essen; Klinik und Poliklinik für Unfallchirurgie [email protected] 29. Florian, Christian Universität Regensburg, Institut für Immunologie [email protected] Universität Erlangen, Institut für Klinische Mikrobiologie, Immunologie und Hygiene Universität Mannheim, Institut für Medizinische Mikrobiologie und Hygiene Universitätsklinikum Bonn, Institut für Medizinische Mikrobiologie, Immunologie und Parasitologie [email protected] Ulm, Medizinische Mikrobiologie und [email protected] [email protected] 30. Friedrich, Diana 31. Geginat, Gernot 32. Gentil, Katrin 33. Gibbert, Kathrin Universitätsklinikum Essen, Institut für Virologie [email protected] 34. Grauling-Halama, Silke Institut für Medizinische Mikrobiologie und Hygiene, Mannheim [email protected] 35. Griewank, Klaus Universität Mainz, Institut für Dermatologie [email protected] 36. Häberlein, Susanne Universität Erlangen, Institut Immunologie und Hygiene 37. Händel, Ulrike Universität Magdeburg, Institut für Medizinische Mikrobiologie [email protected] 38. Haroon, Fahad Universität Magdeburg, Institut für Medizinische Mikrobiologie [email protected] [email protected] für Klinische Mikrobiologie, [email protected] [email protected] [email protected] 40. Heitmann, Lisa Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Forschungszentrum Borstel, Infektionsimmunologie 41. Hölscher, Christoph Forschungszentrum Borstel, Infektionsimmunologie [email protected] 42. Holz, Kristian Forschungszentrum Borstel, Infektionsimmunologie [email protected] 39. Heeg, Klaus [email protected] 43. Jantsch, Jonathan Jugert, Christiane Universität Erlangen, Institut für Klinische Mikrobiologie, Immunologie und Hygiene Universität zu Lübeck; Medizinische Mikrobiologie und Hygiene [email protected] 44. 45. Kalies, Kathrin Universität Lübeck; Institut für Anatomie [email protected] Kaschel, Mariel Esther Universitä Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie [email protected] 46. [email protected] 67 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Name Institute Email 47. Kautz-Neu, Kordula Universität Mainz; Institut für Dermatologie [email protected] 48. Kocur, Magdalena Universität Düsseldorf; Medizinische Mikrobiologie [email protected] 49. Kravets, Elisabeth Universität Düsseldorf, Institut für medizinische Mikrobiologie [email protected] Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Universität Erlangen; Medizinische Mikrobiologie [email protected] 50. Kubatzky, Katharina 51. Lang, Roland 52. Limmer, Andreas Universitätsklinik Bonn; Molekulare Medizin und Experimentelle Immunologie [email protected] 53. Lopez, Susanne Universität Mainz; Institut für Dermatologie [email protected] 54. Lorenz, Beate Universität Mainz; Institut für Dermatologie [email protected] 55. Luhn, Kerstin University of Oxford, John Radcliffe Hospital, MRC Human Immunology Unit [email protected] 56. Masic, Anita Universität Würzburg, Institut für Molekulare Infektionsbiologie [email protected] Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie [email protected] [email protected] 57. Metzdorf, Daniela 58. Minsinger, Andreas 59. Mostböck, Sven Universität Regensburg, Institut für Immunologie [email protected] 60. Munoz, Melba Charite Berlin; Institut für Mikrobiologie [email protected] 61. Neumann, Jan Forschungszentrum Borstel; Mikrobielle Grenzflächenbiologie 62. Nickel, Daniel Universitätsklinikum Hygiene 63. Nippe, Nadine Universität Münster, Institut für Immunologie [email protected] 64. Opitz, Bastian Charite Berlin, Med. Klinik m. S. Infektiologie und Pneumologie, [email protected] Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Universität Duisburg-Essen; Klinik und Poliklinik für Unfallchirurgie [email protected] [email protected] Ulm, Medizinische Mikrobiologie [email protected] [email protected] und [email protected] 65. Parcina, Marijo 66. Pastille, Eva 67. Pfleiderer, Lisa 68. Plickert, Rita Universitätsklinikum Ulm, Medizinische Hygiene Charite Berlin; Institut für Mikrobiologie 69. Raczkowski, Friederike Universitätsklinikum Hamburg Eppendorf, Institut für Immunologie [email protected] 70. Reiling, Norbert Forschungszentrum Borstel; Mikrobielle Grenzflächenbiologie [email protected] 71. Remer, Katharina Universität Würzburg; Molekulare Infektionsbiologie [email protected] 72. Ritter, Uwe Universität Regensburg, Institut für Immunologie [email protected] 73. Schale, Kolja Forschungszentrum Borstel, Mikrobielle Grenzflächenbiologie [email protected] 74. Scheu, Stefanie Universität Düsseldorf; Medizinische Mikrobiologie [email protected] 75. Schleicher, Ulrike Universität Erlangen; Medizinische Mikrobiologie [email protected] 76. Schlüter, Dirk Universität Magdeburg; Medizinische Mikrobiologie [email protected] 77. Schmidt, Kim Universitätsklinik Bonn; Molekulare Medizin und Experimentelle Immunologie [email protected] 78. Schmidt, Lotte Universität Heidelberg; Medizinische Mikrobiologie [email protected] [email protected] Mikrobiologie und [email protected] [email protected] 79. Schnare, Markus 80. Schneider, Bianca Universität Erlangen, Institut für Klinische Mikrobiologie, Immunologie und Hygiene LSHTM London; Infectious and Tropical Diseases 81. Schneider, Michael Universitätsklinikum Hamburg Eppendorf, Institut für Immunologie [email protected] 82. Schneider, Wulf Schoenen, Hanna 84. Schumak, Beatrix Universität Regensburg, Institut für Medizinische Mikrobiologie und Hygiene Universität Erlangen, Institut für Klinische Mikrobiologie, Immunologie und Hygiene Universitätsklinik Bonn; Molekulare Medizin und Experimentelle Immunologie [email protected] 83. 85. Schwandt, Timo Universitätsklinikum Bonn, Institut für Molekulare Medizin und Experimentelle Immunologie [email protected] 86. Schwonberg, Kirsten Universität Mainz, Institut für Dermatologie [email protected] [email protected] [email protected] [email protected] [email protected] 87. Siegfried, Alexandra 88. Sodenkamp, Jan Christian Universität Tübingen, Institut für Medizinische Mikrobiologie und Hygiene Forschungszentrum Borstel; Infektionsimmunologie 89. Stamm, Claudia Universität Lübeck; Institut für Anatomie [email protected] 90. Steinhoff, Ulrich MPI Infektionsbiologie [email protected] Klinikum Virchow, Campus Charite, Berlin, Institut für Neuropathologie Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie [email protected] 91. Stenzel, Werner 92. Strebovsky, Julia 93. Stutz, Andrea [email protected] [email protected] [email protected] 68 13. Symposium "Infektion und Immunabwehr" Burg Rothenfels, 12. – 14. März 2009 Name Institute Email 94. Tschernig, Thomas Medizinische Hochschule Hannover, Institu für Anatomie [email protected] 95. Van Laak, Vincent Charite Berlin, Med. Klinik m. S. Infektiologie und Pneumologie [email protected] 96. Van Zandbergen, Ger Universitätsklinikum Hygiene [email protected] 97. Von Stebut, Esther Universität Mainz, Institut für Dermatologie [email protected] 98. Warnke, Philip Universität Tübingen, Institut für Medizinische Mikrobiologie und Hygiene [email protected] 99. Weighardt, Heike Universität Düsseldorf, Institut für umweltmedizinische Foschung [email protected] 100. Wirsdörfer, Florian Universitätsklinikum Essen, Klinik für Unfallchirurgie [email protected] Wölfle, Sabine Universität Heidelberg, Institut für Hygiene und Medizinische Mikrobiologie [email protected] 101. Ulm; Medizinische Mikrobiologie und 69