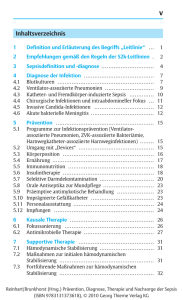
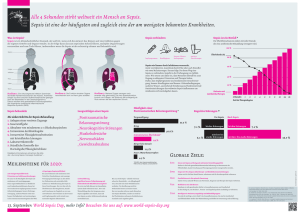
Sepsis Pathophysiologie - Diagnose - Therapie Sepsis
Werbung

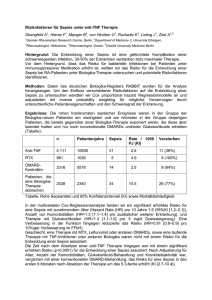
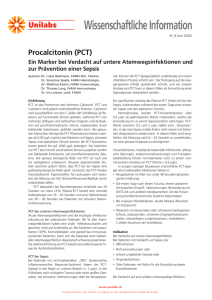
09.05.2012 Kantonsspital Aarau Medizinische Universitätsklinik Sepsis Pathophysiologie - Diagnose - Therapie Prof. Dr. med. Beat Müller Dank an Dr. Marc Michot, medIPS, KSA Sepsis - Fallvignette • 73j. M, Raucher, täglich Gartenarbeiten • Seit 2 Tagen rechtsthorakale Schmerzen u. zunehmende Dyspnoe, etwas Fieber • Akute Dyspnoe am Eintrittstag • Rettung: bradykarder Rhythmus DD: PEA kurze mechan. REA Intubation vor Ort • INZ: RR 70/40mmHg 31. Mai 2012 14 3.9 10 1 09.05.2012 SEPSIS Sepsis-Inzidenz Vergleich mit anderen Erkrankungen Zukunft Heute 110 / 100.000 Einw.1 Brustkrebs •Steigende Zahl älterer Mitbürger •Lebenserhaltende Technologie > Mio Fälle schwerer Sepsis* •Invasive Techniken •Nosokomiale Infektionen •Antibiotika-Resistenz *OECD = Organization for Economic Cooperation and Development Linde-Zwirble et al. Crit Care Med 1999; 27: A33 Opal und Cohen, Crit Care Med 1999; 27: 1608 Sepsis ! häufig 1 2 Kolonkarzinom 50 / 100.000 Einw.1 AIDS schwere Sepsis Sepsis 17 / 100.000 Einw.1 300 / 100.000 Einw.1 240 / 100.000 Einw.2 Angus DC et al; Crit Care Med 2001; 29: 1303-1310 Martin GS et al, N Engl J Med 2003;348:1546-54 Pathophysiology of Severe Sepsis Endothelium tödlicher als andere Akuterkrankungen verursacht die höchsten Kosten auf IPS COAGULATION CASCADE IL-6 IL-1 TNF- Factor Va Monocyte unterschätzt in der öffentlichen Wahrnehmung TAFI THROMBIN Fibrin clot Neutrophil Tissue Factor Moerer O et al.,Intensive Care Med 2002; 28: 1440-1446 - Leucocyte Activation -> Cyotokine storm PAI-1 Clotting -> DIC - Second. Organ Failure -> Severe Sepsis Suppressed - Vasodilation & fibrinolysis Permeability -> Shock Factor VIIIa - Tissue Factor Organisms Effects Inflammatory Response to Infection Fibrin IL-6 Thrombotic Response to Infection Fibrinolytic Response to Infection Adaptiert von Bernard GR, et al. New Engl J Med 2001;344:699-709. 2 09.05.2012 Progrediente „Sepsis“ Infektion/ Trauma SIRS Sepsis Severe Sepsis Markers of Acute Organ Dysfunction Schwere Sepsis Altered Consciousness Confusion Psychosis Tachycardia Hypotension CVP PAOP Sepsis mit 1 Organversagen: Tachypnea PaO2< 70 mm Hg SaO2 < 90% PaO2/FiO2 300 Respiratorisch ZNS Oliguria (≤0.5ml/kgKG/h) Anuria Creatinine Kardiovaskulär Hepatisch Renal Schock Gerinnung Metabolische Azidose Jaundice Enzymes Albumin PT Platelets PT/APTT Protein C D-dimer Lactatacidosis (pH < 7.3 or Lactat ≥ 1.5 of norm) ACCP/SCCM Consensus. Crit Care Med 1992; 20(6): 864-874. Gesunde Person mit Meningokokken-Sepsis Alter Patient mit Malnutrition und Divertikulitis Patient mit Diabetes, chronischem Nierenversagen und Pneumonie Cytokines & Hormokines upon Infection TNFa IL6 PCT CRP ug/ml 5 Fatal Outcome normal 4 3 Erholung hypoimmun Immunstatus hyperimmun Immunantwort bei Patienten mit Sepsis 2 1 Tod Tage 1 2 3 4 5 6 7 0 8 Hotchkiss et al. New Engl J Med 2003; 348: 138-150 Guertler C., et al. Eur Resp J 2011; 2011; 37: 1439–1446 Editorial: Mortensen E.M. Eur Respir J 2011; 37: 1306–1307 Sepsis - Diagnose 0 Endotoxin iv 12 24 36 48 60 72 h adapted from Meisner M, J Lab Med Dandona P, et al. J Clin Endocrinol Metab Harbarth S, AJRCCM Becker KL, J Clin Endocrinol Metab 1999 1994 2001 2004 Sepsis - TIME IS LIFE ! 3 09.05.2012 Sepsis: Kombination von Infektion & Inflammation Infektion/ Trauma SIRS* Sepsis ? Schwere Sepsis Eine klinische Reaktion auf einen SIRS mit angenommener nicht-spezifischen Insult, die 2 oder oder nachgewiesener mehr der folgenden Symptome Infektion aufweist: Temperatur 38°C oder 36°C Herzfrequenz 90 /min Atemfrequenz 20/min od.pCO2<32 Leukozyten 12.000/mm3 oder 4000/mm3 oder > 10 % unreife Neutrophile *SIRS = Systemisches Inflammatorisches Reaktionssyndrom (engl.: “systemic inflammatory response syndrome“) ACCP/SCCM Consensus Conference Committee. Chest 1992; 101:1644-55 ACCP/SCCM Consensus Conference Committee. Crit Care Med 1992; 20(6): 864-874. PIRO System for Staging Sepsis 2001 SCCM/ESICM/ATS/SIS INTERNATIONAL SEPSIS DEFINITIONS CONFERENCE , >100 infection and sepsis markers proposed , For the Sepsis Definitions Conference: Abraham E, Angus D, Cohen J, Cook C Fink M Levy MM, Marshall J, Ramsay G, Reinhart K, Marshall J, Opal S, Vincent J-L Gegenwart Zukunft Prädisposition Vorerkrankungen Genetische Polymorphismen Infektion Kulturen Mikrobielle Produkte (LPS,mannan,DNA) Response SIRS Biomarkers: PCT, Il-6, TNF, PAF, aProtein C..... Immunität : HLA-DR, ... Organdysfunktion Scores: SOFA, MODS dynamisch: Zellantwort auf Insult: Apoptose, Zellstress, cytopath. Hypoxie Levy MM et al. Intensive Care Med (2003) 29:530.538 „Hormokines“ Hormones expressed like Cytokines Why Procalcitonin? Healthy Sepsis PCT 1 Thyroid Leukocytes Perit. Macrophages Spleen 1 Lung Liver Kidney Adrenals Brain Spine Sensitivity Sensitivity CRP IL-6 Stomach Pancreas Small Intestine PCT + Clinical Diagnosis Lactate Clinical Diagnosis alone 0 Thyrocytes 0 0 1- Specificity 1 Colon C-Cells Heart 0 1- Specificity 1 Thyroxine Calcitonin et Asn Le u Ser Gly Cy s ArgLy s Ser Gly Glu Arg Glu Gln G u l Gn l Glu Leu Glu Ser Ala Ser Arg Pr o Ser Asp Le u Se r Lys Calcitonin SH SH l Thr Cys M et Le u Gly Thr Ty r Thr Gln As p Phe Asn Ly s Phe His Thr Phe Pro Gln Thr Ala Ile G y Va l Gly Müller B, Crit Care Med (2000) 28:977-983 Harbarth S, Am J Respir Crit Care Med (2001) 164:396-402 CCP- I ( Katacalcin) Ala Asn Gln Ala Inflammation Bacterial Interferons Toxins viral IL-1 Infection TNF Procalcitonin Ala Le u 1 14 Ser Ar g Phe Pr o Ala - NH2 Glu Leu Ser Glu Asp Glu Ala Ar g L eu L eu Leu Ala Ser Ser Pr o Ala Asp Pr o Ala T hr Ala Leu Val G ln Asp Tyr Val Gln Aminoprocalcitonin Pro Se r Asp L eu Se r Ser Gly Glu Ar g Glu G ln Gl u Gln Glu Le u G lu Ser Ala L ys Ser Arg Asn Gly Cy s Ar g Leu SH SH Me t Lys Calcitonin Ser Th r Cys M et Leu Gl y Th r T yr T hr G ln Asp Phe Asn Ly s Ph e His Th r Ph e Pro Gl n T hr Al a Ile Gly Val Gly CCP-I (Katacalcin) Ala Asn CO OH- Ala Pr o Pro Met Ser Val His Pro Ar g His As p Ar g Glu Leu Asp Ser Se r Me t As p Ar g Ly s Lys Gly Asn Gl n Muscle Skin Adipose Tissue Testes Pro Pro Me t Ser Va l His Pro Ar g His As p Arg Glu Le u As p Ser Se r Me t As p Arg Ly s Lys Gly Müller B, et al. J Clin Endocrinol Metab 2001 4 09.05.2012 Therapie Door-to-Action-Time „Unfortunately, there‘s no cure, there‘s not even a race for a cure.“ The New Yorker, July 98 Tödliche Verzögerung einer adäquaten Therapie Early goal directed therapy • Früher und aggressiver Therapie-Beginn ist entscheidend (Ziel: Ausgleich von O2-Angebot (DO2) und O2- Nachfrage (VO2) innert 6h) • Start der Sepsis-Kaskade kann vermindert / verhindert werden (vgl frühere Studien: sobald Sepsis Kaskade läuft, ist aggressive Hämodynamikkorrektur sogar kontraproduktiv) Kumar A, Crit Care Med 2006;34: 1589-96 Early Goal-Directed Therapy O2-Insufflation bzw. Sedierung Intubation + Beatmung Early Goal-directed Therapy bei schwerer Sepsis und septischem Schock: Outcome • Monozenter, RCT, 263 Pat. Zentraler Venenkatheter Invasive Blutdruckmessung Letalität • schwere Sepsis od. sept. Schock Kreislaufstabilisierung Krankenhaus 6h ZVD <8mmHg LOS Vasopressoren p=0.009 49,2 30.5 Beatmung Volumentherapie 8-12 mmHg P=0.01 33.3 28-Tage 49.2 Krankenhaus <65 mmHg MAP Vasopressoren 65 mmHg Bluttransfusion bis Hämatokrit 30% 70% Ziel erreicht? ScVO2 <70% Inotropika 70% ja P=0.03 44.3 56.9 60-Tage <70% ScVO2 nein * p < 0.05 46.5 Therapie beibehalten, regelmäßige Neuevaluierung Rivers E et al. New Engl J Med 2001;345:1368-77 0 10 30 50 70 * Krankenhaus survivors 0 5 10 15 20 Tage Patienten (%) EGDT Standard Rivers E et al. New Engl J Med 2001;345:1368-77 5 09.05.2012 Early Goal-directed Therapy bei schwerer Sepsis und septischem Schock: Interventionen Interventionen erste 6 Std. * Vasopressor SBP <90 mmHg oder MAP <65 mmHG nach 20-30 ml/kg Kristalloid i.v. -oderLactat > 4 mmol/l Volumen (Liter) 12 Ery-Konz. Schwere Sepsis / Septischer Schock: Early Goal Directed Therapy (EGDT) – Protokoll KSA Sauerstoff Einlage ZVK und arterieller Katheter +/- endotracheale Intubation und mechanische Ventilation (wenn notwendig) gleichzeitig Weiterführen der i.v.Resuscitation mit Kristalloiden / Kolloiden (500-1000ml Bolus) (3-lum ig) <8 mmHg 8 * 4 Beatmung PAK 0 10 30 50 70 0 0-6 h Patienten (%) Rivers E et al. New Engl J Med 2001;345:1368-77 Infektionsherd / Erreger 7-72 h Aktivierung der Abwehrzellen Primäre Mediatoren ( TNF, IL, PAF ) Disseminierte intravasale Gerinnung Klinische Auswirkungen -Kardiozirkulation -Mikrozirkulation ARDS, ANV, DIC Leberversagen Das Protokoll soll innert 1h nach Diagnosestellung begonnen werden. 8-12 mmHg Therapie nach Protokoll während den ersten 6h . ≥65 mmHg <65 mmHg Vasopressoren (Noradrenalin bevorzugt) MAP <70% ScvO2 †† Wenn PA-Katheter eingeführt, PCWP Ziel 12-15 mmHg (ersetzt ZVD-Ziel) und SvO2>75 % (ersetzt ScvO2Ziel). Standard * p < 0.001 >70% Transfusion von Erythrozyten Hb > 70g/l ≥70% <70% Inotropika (Dobutrex bevorzugt) Erstrebte Ziele ? Nein Ja EGDT Michot / MIPS / KSA 2006 Herdsanierung / Antibiotika Antitoxine ? Toxinelimination (Toraymycin®) Toxine Kristalloid / Kolloid i.v. ZVD * Inotropika Information Medizinische Intensivstation Immunglobuline O2-Radikalfänger Pentoxifylline ? ? ? Anti-TNF-AK TNFra ILra Anti-PAF-AK PAF-acetylhydrolase ? ? ? ? ? Aktiviertes Protein C (Xigris®) Tissue Factor Pathway Inhibitor Antithrombin III ? ? Therapie beibehalten, regelmässige Neuevaluation Herdsanierung / Antibiotika Infektfokus suchen Kultivieren Antibiotika Sanieren Intensivmedizin - Schockbehandlung: EGDT - Beatmung: Tidalvolumina / PEEP - (RNNI: Cortisolsubstitution) - (Glc-Homöostase: Insulinsubstitution) Why is a critically-ill medical patient “septic”? Biomarker guided therapy in the ICU „Bacterial“ Sepsis ≈ 65% organism known, <50% pos BC „Bacterial“ CAP ≈ 30% organism known, ≈ 10% pos BC ? Signs & Symptoms? Temperature, BP - SIRS criteria Imaging? Cultures? - Blood, Sputum, Tissue Laboratory? - Leukocytes / WBC - ESR, CRP, SAA - Neopterin, sTREM-1 Other? others Brain CardioVascular Dyspnea (AECB…) Sepsis 33% Pneumonia 67% Condition Diabetes Hyperglycemia Hypotension Shock Infection Sepsis ‘Biomarker’ Blood glucose Lactate / ScvO2 Procalcitonin?! UTI GIT others Treatment Insulin: Fluid: Antibiotics Dose / type Amount / rate Initiation / duration Müller B, Crit Care Med 2000; 28: 977-83 Christ-Crain M, AJRCCM, 06; 174: 84-93 6 09.05.2012 The PROBABILITY for worsening of bacterial infections increases with Procalcitonin-levels Risk-adapted Antibiotic Therapy ? Amino-ProCT (ng/mL; n=651) 100 Hausarzt! “Overruling” ? (“Gatekeeper”) (High-risk, Co-Morbidities) 10 Diagnosis Respiratory Infection? Therapy Antibiotics ? Clinical Exam Procalcitonin (pivotal & valuable!) (“Biomarker”) “Medicine is the science of uncertainty 1 and the art of probability.” Sir William Osler, 1902 0.1 Signs & Symptoms 0.01 Reconval. SIRS Sepsis Severe Sepsis . Septic Shock Cultur, serology Radio ‐logy <0.1 Acute COPD CAP STOP Bronchitis Exazerbation Pneumonia Antibiotics 0.1‐0.25 0.26‐0.5 Stop/Start based on Algorithm ≥0.5 START Antibiotics Müller B, Crit Care Med 2000 Guide of antibiotic Therapy: Proof-of-Concept RCTs Overview of PCT Intervention studies for Antibiotic Stewardship (n=4467) Respiratory Tract Infection Standard Group (without PCT-result) PCT Group Randomization PCT Treatment Based on Standard Guidelines Follow-up After 10-14 Days Antimicrobial Treatment <0.1 NO! 0.1-0.25 No 0.25-0.5 Yes >0.5 YES! Clinical and PCT Control After 6-24h (ng/ml) PCT for Antibiotic Stewardship in the ICU ? Schuetz P, et al Arch Intern Med 2011; 171: 1322-31 Schuetz P., et al Clin Inf Dis 2012 (in press) Cochrane Database 2013 (submitted) Procalcitonin for antibiotic stewardship in other sites of infections? Meningitis Sepsis Endocarditis Respiratory tract infections UTI Abdominal infections e.g. Pancreatitis, Diverticulitis Arthritis Osteomyelitis 7 09.05.2012 Limitations in the ICU setting The PRORATA Study: Multicenter, ICU, Sepsis n = 621 • Low adherence to algorithm (around 50%) – PCT does not replace clinical intuition Antibiotic Duration • Main focus CAP/ED, mostly European Outcome – Future research is needed to valdiate this concept in the ICU setting • False positives & negative values occur – pos: Surgery, cardiac shock, „cytokine storm“,… – neg: early, localised, subacute… – ICU: Guide duration, rather than prescription • „Single“ PCT measurement is of limited value – Consider the course of PCT over time 23% more antibiotic free days alive Bouadma, Lancet 2010 The PRORATA Study – Subgroups Antibiotic Duration Guidelines (2011 / 2012) Outcome “ …Recently, biomarkers have been described as useful tools to safely reduce antibiotic treatment duration. Biomarkers can guide treatment duration by the application of predefined stopping rules for antibiotics. It has been shown that such rules work even in most severe cases, including pneumonia with septic shock, and even if clinicians are allowed to overrule the predefined stopping rule … “ Woodhead, Clin Microbiol Infect 2011; 17(Suppl. 6): E1–E59 “We suggest the use of low procalcitonin to assist the clinician in the discontinuation of empiric antibiotics when no evidence of infection is found (grade 2C)” Update Surviving Sepsis Campaign, Dellinger P., SCCM, Houston 2012 Bouadma, Lancet 2010 If the Swiss would rule the world ... If PCT would rule the world ... Procalcitonin Guided Antibiotic Therapy 90%? Clinical Skills ! Guidelines ! RTI Setting „Common Cold“ Primary Care Bronchitis Emergency Room Pneumonia Hospital Mortality <<1% <1-3% 5-20% 30-70% AB-Initiation Duration AB exposure 75% 44% 40% 0% 106d 75% 44% 40% 14% 125d 64% The less antibiotic exposure, the less resistance & side-effects ! Education ! Sepsis ICU 40% Christ-Crain et al., Lancet 04 Christ-Crain et al., AJRCCM 06 & 08 Stolz et al., CHEST 07 Nobre, AJRCCM 07 Briel et al., Arch Int Med 08 Schütz et al., JAMA 09 Stolz et al., ERJ 2010 Bouadma, Lancet 2010 (Re)-Enforcement ! 50% USA! PCT There‘s no business like health business! Filippini M, Health Policy, 2006 8 09.05.2012 Worldwide epidemic of resistant bacteria Why ? Because we (mis)use antibiotics !! MRSA Grundmann et al. Lancet 2006; 368: 874-85 9