Innate immunity - Paul-Ehrlich
Werbung
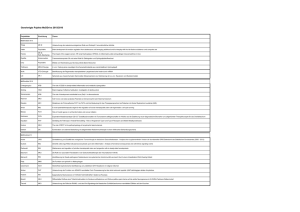
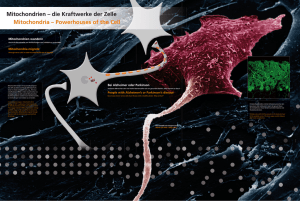
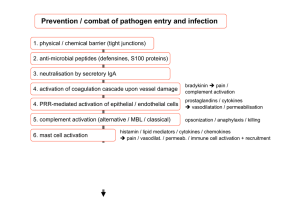
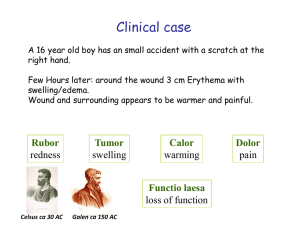
Innate immunity [email protected] Paul-Ehrlich-Institut Paul-Ehrlich-Institut Bundesinstitut für Impfstoffe und biomedizinische Arzneimittel Wettrüsten zwischen Wirt und Virus Evolution Anti-virales Wirtsmolekül Virales Molekül Virus // lution Evolution Slide adapted from Carsten Münk „Hierzulande musst du so schnell rennen, wie du kannst, wenn du am gleichen Fleck bleiben willst. Um woandershin zu kommen, musst du mindestens doppelt so schnell laufen!“ The Red Queen to Alice in Alice in Wonderland SM. Hedrick 2004 Slide adapted from Carsten Münk Das Immunsystem als Hürde für die Virus-Ausbreitung Intrinsische Immunität Angeborene Immunität Erworbene Immunität Flint, Principles of Virology, 2009 Das Immunsystem als Hürde für die Virus-Ausbreitung Intrinsische Immunität Angeborene Immunität Erworbene Immunität Flint, Principles of Virology, 2009 Intrinsic defenses • Barriers (e.g. skin, normal flora, …) • Apoptosis (“altruistic suicide”) • Autophagy (“eating in to avoid infection”) • Epigenetic silencing (defense against DNA viruses replicating in the nucleus) • RNA silencing (sequence-specific degradation of virus RNA) • Cytosin deamination (Apobec affecting RT of retroviruses) • Trim Proteins (protection against endemic retroviruses) Intrinsic barriers to infection Skin Gut Lungs Eyes/Nose Apoptosis upon viral infections At the cell surface: • Induction of apoptosis-inducing cytokines • Alteration of membrane integrity In the cytoplasm: • Production of metabolic inhibitors • Modification of cytoskeleton Infection of human epithelial cells with HSV-1 results in membrane blebbing and apoptotic body formation In the nucleus: • Damage to DNA • Alteration of gene expression • Disruption of cell cycle Adapted from Flint, Principles of Virology, 2009 Autophagy disposing invaders without disposing the whole cell Levine et al., 2007 Nature Reviews Das Immunsystem als Hürde für die Virus-Ausbreitung Intrinsische Immunität Angeborene Immunität Erworbene Immunität Flint, Principles of Virology, 2009 Innate immune responses C • Complement (classical pathway, lectin pathway, alternative pathway) • Innate immune cells (e.g. dendritic cells, NK cells, …) IFN • Cytokines (e.g. type I interferons) Innate immune responses C • Complement (classical pathway, lectin pathway, alternative pathway) • Innate immune cells (e.g. dendritic cells, NK cells, …) IFN • Cytokines (e.g. type I interferons) Cells of the innate immunity Macrophage • Phagocytosis and activation of bactericidal mechanisms • Antigen presentation Neutrophil • Phagocytosis and activation of bactericidal mechanisms Dendritic cell • Phagocytosis • Antigen presentation Eosinophil • Killing of antibody-coated parasites NK cell • Release of lytic granules that kill virus-infected cells Basophil • Unknown Mast cell • Release of granules containing histamine and other active agents Dendritic cells detect „foreign“ • Detect PAMPs (pathogen associated molecular patterns) via PRRs (pattern recognition receptors) • Sentinel cells “show” the pathogen on MHC II to cells of the adaptive immunity • Get activated in periphery and mature (MHC II upregulation, upregulation of costimmulatory molecules, cytokine release) • Migrate to secondary lymphatic organs • Initiate adaptive immune response Flint, Principles of Virology, 2009 Natural killer cells detect „missing self“ • “Dynamic equilibrium concept” • Inhibition of NK cells by detecting MHC I molecules • Activation of NK cells by “alert molecules” (self and non-self) • Release perforins and granzymes perforating membranes and trigger caspase-mediated cell-death • Produce IFN- • Antibody-dependent cell cytotoxicity (ADCC) via Fc receptor CD16 Vivier et al., 2008 Nature Reviews Viral mechanisms for modulation of NK cell activity 1. Expression of viral MHC I homolog by infected cell (HCMV UL18) 2. Increase of host HLA-E expression (Nef of HIV1 affects MHC I expression, but not of MHC I E) 3. Expression of viral activating receptor antagonists (HCMV E2 envelope protein binding to CD81) 4. Catch NK cell stimulatory cytokines or produce cytokine agonists (Ectromelia encoded IL-18 binding protein inhibits IFN- production) 5. Infection of NK cell itself Adapted from Flint, Principles of Virology, 2009 Innate immune responses C • Complement (classical pathway, lectin pathway, alternative pathway) • Innate immune cells (e.g. dendritic cells, NK cells, …) IFN • Cytokines (e.g. type I interferons) Immunantwort nach Kontakt mit einem Pathogen - Viren - Bakterien - Protozoen - Parasiten Interferone IgM Killer Zellen IgG Tage nach Infektion 4 Angeborene Immunität 8 Erworbene Immunität 12 Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Interferone sichern das Überleben nach Infektion Interferon IgM Killer IgG Überleben Wild-typ Maus 4 8 12 Überleben Maus ohne Killer Zellen 4 8 12 Überleben Maus ohne Antikörper-produzierende Zellen 4 8 12 Überleben Maus ohne Typ I Interferon System 4 8 12 VSV Type I, II, and III interferons Type I interferons Type II interferon IFN- IFN-/ IFNAR IFNGR Type III interferons IFN-1-3 IFNLR Mechanism of IFN- induction IFN- IFNAR IFN- IRF-3 STAT JAK NF-B IRF-7 IFN- Type I IFN-mediated anti-viral effects Virus-infected host cell • Induction of 2’-5’ oligoadenylate synthetase - Activation of an endoribonuclease - Degradation of viral RNA • Induction of P1-kinase (serine/threonine kinase) - Inhibition of translation - Inhibition of viral replication IFN- and IFN- expression >300 target genes • Induction of Mx - Mediates resistance against influenza infection - Targets viral nucleocapsids - Inhibits RNA sythesis • Induction of protein kinase R - dsRNA-dependent - Inhibits translation initiation •… Interferone in klinischen Anwendungen Zulassungen Datum Handelsname Wirkstoff Hersteller Indikation 1983 Fiblaferon® IFN beta Rentschler Schwere Viruserkrankungen / 2003 SARS 04/1987 Roferon A® IFN alpha-2a Roche Krebs 11/1995 Betaferon® IFN beta-1b Schering Multiple Sklerose 03/1997 Avonex® IFN beta-1a Biogen Multiple Sklerose 05/1998 Rebif® IFN beta-1a Serono Multiple Sklerose 02/1999 Inferax® IFN alphacon 1 Yamanouchi Hepatitis C 03/2000 Intron A® IFN alpha-2b Essex Pharma Hepatitis B/C 02/2002 PegIntron® pegyliertes IFN alpha-2b Essex Pharma Hepatitis C 06/2002 Pegasys® pegyliertes IFN alpha-2a Roche Hepatitis B/C 10/2007 CinnoVex® biogeneric IFN beta-1a CinnaGen Multiple Sklerose 06/2008 Extavia® IFN beta-1b Novartis Multiple Sklerose (identisch mit Betaferon®) Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Identification of interferon producing cells in the spleen VSV Immunohistochemistry: anti IFN- antibody Barchet et al. (2002), JEM FACS-sorting of dendritic cell populations 1. VSV infection in vivo 4. FACS analysis and FACS-sorting VSV C 2. Suspension of spleen cells CD11c A D B E C/D GR-1 F CD11b 3. MACS pre-sort for CD11c+ cells A: Lymphoid DC (CD11c+CD11b-); CD8+ DC B: Myeloid DC (CD11c+CD11b+) C: GR-1- DC (CD11cintCD11b-GR-1-) D: GR-1+ DC (CD11cintCD11b-GR-1+) E: Macrophage-like DC (CD11cintCD11b+) F: Granulocytes (GR1+) Barchet et al. (2002), JEM Identification of plasmacytoid dendritic cells as IFN- source in the spleen IFN- RT-PCR untreated C CD11c A VSV D B E C/D GR-1 F CD11b Barchet et al. (2002), JEM Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Classification of cytokines Functional group Selected members Activity Pro-inflammatory cytokines IL-1, TNF-, IL-6, IL-12 Promote leukocyte activation Anti-inflammatory cytokines IL-10 Suppress activity of pro-inflammatory cytokines; return system to basal “circulate and wait” state Chemokines IL-8 Recruit immune cells during early stages of immune response Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Massive fungal infection in Toll-/- fruit flies Lemaitre et al. (1996), Cell How do DC sense pathogens? 1996 Spätzle/Toll/cactus control potent antifungal response in Drosophila (Lemaitre et al., Cell) 1998 Positional cloning of LPS resistance in C3H/HeJ mice revealed that LPS is recognized by TLR4 (Poltorak et al., Science) Toll-like receptors (TLRs) PRR: pattern recognition receptors PAMPs: pathogen associated molecular patterns LRR extracellular cytoplasm TIR domain MyD88 TRIF TLR-dependent and -independent pathogen recognition bacterial lipoproteins LPS PLP Flagellin ? TLR2 TLR6/1 TLR4 TLR5 TLR10, 12, 13 TLR11 extracellular cytoplasm PPP TLR3 TLR7/8 dsRNA ssRNA dsDNA RIG-I MDA5 DAI TLR9 endosome ? PKR TLR signaling …updated July 2004 updated September 2005 updated October 2005 updated March 2008 updated …….. Pattern-recognition receptors expressed by human DC subsets Kadowaki et al. (2001) PAMPs trigger cytokine production LTA (TLR2) LPS (TLR2/4) CpG (TLR9/DAI?) poly I:C (TLR3/RLH) pDC imDC mono. pDC imDC mono. pDC imDC mono. pDC imDC mono. pDC imDC mono. IL-12 INF- IL-6 TNF- PGN (TLR2) Kadowaki et al. (2001) Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Ausschüttung von Interferon nach Kontakt mit einem Pathogen Interferon Type I IFN-mediated effects on adaptive immunity??? IgM IgG CTL response IFN-I days post infection 4 Innate immunity 8 Adaptive immunity 12 IFNAR-dependent antibody class switch VSV-VLP Antibody class switch? WT or IFNAR-/- Bach et al. (2005) Type I IFN-mediated effects on adaptive immunity??? IgM IgG CTL response IFN-I days post infection 4 Innate immunity 8 Adaptive immunity 12 IFNAR-dependent T cell expansion WT IFNAR-/- T cell expansion? IFN % transferred T cells of CD8+ T cell 30 MVAgp33 WT IFNAR-/- Development - Activation - Proliferation + Expansion + Survival + Function + 20 10 0 3 4 5 days post infection 6 7 Frenz et al., 2010 Bridging innate and adaptive immunity IFN-/ 4 2 1 3 pDC 6 5 n mDC X CD8+ T cell B cell IgM Clearance of viral infection IgG Paul-Ehrlich-Institut Bundesinstitut für Impfstoffe und biomedizinische Arzneimittel Literature ISBN: 1555814794 ISBN: 3-8274-2047-4 ISBN: 978-1-904455-81-3