Beckwith-Wiedemann syndrome Hypoglossal nerve injury Lingual
Werbung
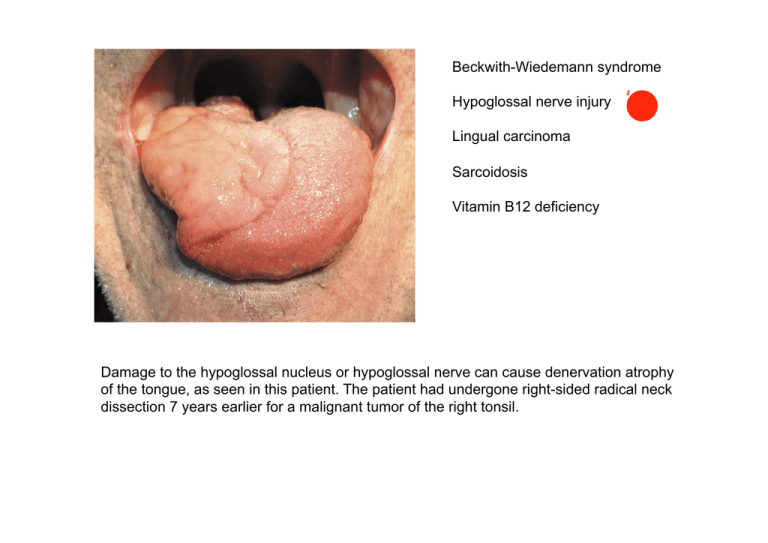
Beckwith-Wiedemann syndrome Hypoglossal nerve injury Lingual carcinoma Sarcoidosis Vitamin B12 deficiency Damage to the hypoglossal nucleus or hypoglossal nerve can cause denervation atrophy of the tongue, as seen in this patient. The patient had undergone right-sided radical neck dissection 7 years earlier for a malignant tumor of the right tonsil. Young child with BeckwithWiedemann syndrome. Note the macroglossia, prominent eyes, eyelid nevus flammeus and barely visible linear ear creases. Note the wasted left side of the tongue and deviation to the left suggesting a left lower motor neurone lesion. Thrombopoetin oder auch Thrombopoietin (Gen-Name: THPO) ist ein Hormon, das die Bildung und Differenzierung der Blutplättchen-bildenden Zellen, der Megakaryozyten, stimuliert. Es ist im Rahmen der Thrombopoese notwendig für die Produktion von Blutplättchen (Thrombozyten). Mutationen im THPO-Gen können zu (seltener) erblicher Thrombozythämie führen. Thrombopoetin wird in der Leber, der Niere, sowie in den Stromazellen des Knochenmarks gebildet. Es nimmt an verschiedenen Stellen Einfluss auf den Ablauf der Hämatopoese und wirkt dabei als Cytokin. Neben dem Einfluss auf Megakaryozyten und der einhergehenden Bildung der Thrombozyten wirkt Thrombopoetin auf hämatopoetische Stammzellen. Bei Eltrombopag handelt es sich um einen nicht-peptidischen, oral aktiven ThrombopoetinRezeptor-Agonisten. Dieser Wirkstoff stimuliert die Proliferation und Differenzierung von Megakaryozyten – den Vorläuferzellen der Thrombozyten (Blutplättchen) – was zu einer Erhöhung der Blutplättchenkonzentration führt. Die Resultate einer klinischen Phase-III-Studie zeigten, dass bei den 114 Probanden mit idiopathischer thrombozytopenischer Purpura die tägliche, orale Gabe von 50 mg Eltrombopag zu einem deutlichen Anstieg der Anzahl Blutplättchen führte. Bei 80 % der Patienten, die Eltrombopag erhalten, treten Nebenwirkungen auf. Dies sind hauptsächlich Kopfschmerzen, gastrointestinale Störungen (z.B. Übelkeit, Durchfall, Erbrechen), Schlaflosigkeit, Augentrockenheit und Hautausschlag. Schwerwiegende Nebenwirkungen wurden keine beobachtet. Die positiven Resultate der Phase-II-Studien wurden 2007 bereits publiziert. Eltrombopag and Improved Hematopoiesis in Refractory Aplastic Anemia We conducted a phase 2 study involving patients with aplastic anemia that was refractory to immunosuppression to determine whether the oral thrombopoietin mimetic eltrombopag (Promacta) can improve blood counts. Twenty-five patients received eltrombopag at a dose of 50 mg, which could be increased, as needed, to a maximum dose of 150 mg daily, for a total of 12 weeks. Primary end points were clinically significant changes in blood counts or transfusion independence. Patients with a response continued to receive eltrombopag. The Venn diagrams show the numbers of patients with unilineage, bilineage, and trilineage hematologic responses. Patients with a response and their response pattern at 12 weeks are shown on the left. Patients who met the response criteria at the most recent follow-up assessment are shown on the right. Treatment with eltrombopag was associated with multilineage clinical responses in some patients with refractory severe aplastic anemia. Renale Clearance bezeichnet die Clearance durch die Nieren, d. h. die Entfernung einer bestimmten exogenen oder endogenen Substanz aus dem Blut als spezifische Leistung der Nieren und gibt das Plasmavolumen an, welches pro Zeiteinheit von der entsprechenden Substanz befreit wird. So z. B. für die Kreatinin-Clearance: Die einfache Version der Cockcroft-Gault-Formel hilft, die Kreatinin-Clearance [ml/min] zu schätzen. The Modification of Diet in Renal Disease (MDRD) Study was the largest randomized clinical trial to test the hypothesis that protein restriction slows the progression of chronic renal disease. However, the primary results published in 1994 were not conclusive with regard to the efficacy of this intervention. Cystatin C (auch: CysC) ist ein körpereigenes Protein, das in der Nierendiagnostik zur Bestimmung der glomerulären Filtrationsrate (GFR) verwendet wird. Die Serum-Normalwerte beim Menschen liegen für beide Geschlechter zwischen 0,53 und 0,95 mg/l. Erhöhte Werte finden sich bei eingeschränkter glomerulärer Filtrationsrate (GFR). Cystatin C ist Mitglied der Cystatin-Familie der Cysteinproteasen-Inhibitoren. Cystatin C wird von den meisten kernhaltigen Zellen in relativ konstanter Rate produziert; die Produktion scheint auch bei entzündlichen Prozessen und anderen pathologischen Zuständen gleich zu bleiben. Seltene Mutationen im CST3-Gen können erbliche Amyloidose und Makuladegeneration verursachen. Bei nicht möglicher 24-stündiger Urinsammlung für eine renale Clearance-Bestimmung ist Cystatin C im Serum eine Alternative zur Diagnostik von Störungen der glomerulären Filtration. Durch die größere diagnostische Sensitivität als Kreatinin im Serum scheint es auch Aussagen im „Kreatinin-blinden Bereich“ zuzulassen. Kreatinin = 0,40 € Cystatin C = 4,0 € Estimating Glomerular Filtration Rate from Serum Creatinine and Cystatin C Estimates of glomerular filtration rate (GFR) that are based on serum creatinine are routinely used; however, they are imprecise, potentially leading to the overdiagnosis of chronic kidney disease. Cystatin C is an alternative filtration marker for estimating GFR. Using cross-sectional analyses, we developed estimating equations based on cystatin C alone and in combination with creatinine in diverse populations totaling 5352 participants from 13 studies. These equations were then validated in 1119 participants from 5 different studies in which GFR had been measured. Cystatin and creatinine assays were traceable to primary reference materials. Bias was assessed as the median of the difference between measured GFR and estimated GFR, and precision was assessed as the interquartile range for the difference. Accuracy was assessed as the root-mean-square error and as the percentage of estimates that differed by more than 30% from the measured GFR (1–P30) or by more than 20% (1–P20). Confidence intervals were calculated by means of bootstrap methods (2000 bootstraps). The significance of the differences among equations was determined with the use of the signed-rank test for bias, the bootstrap method for the interquartile range and root-mean-square error from the 2000 bootstrap samples, and McNemar's test for 1–P30 and 1–P20. A reduction in GFR to less than 60 ml per minute per 1.73 m2 for 3 months or longer is a diagnostic criterion for chronic kidney disease and is associated with an increased risk of adverse outcomes, including death. Bias with the new, combined creatinine–cystatin C equation and with the average of the new cystatin C equation and the creatinine equation was similar to that with the individual creatinine and cystatin C equations, but they had greater precision and accuracy and resulted in more accurate classification of measured GFR as less than 60 ml per minute per 1.73 m2 — the threshold for the diagnosis of chronic kidney disease. 3.6% of U.S. adults would be classified as having chronic kidney disease solely on the basis of a creatinine-based GFR estimate of 45 to 59 ml per minute per 1.73 m2. Our data suggest that a strategy of measuring cystatin C when the creatinine-based estimate is in this range and then reestimating GFR with the use of both these markers could correctly reclassify a substantial proportion of such patients as not having chronic kidney disease and not being at high risk. This more accurate classification would result in more selective use of resources, such as tests for complications of chronic kidney disease, adjustment of medication doses, and referrals to nephrologists. Delirium ist ein akutes, schweres, prinzipiell reversibles, organisch bedingtes Psychosyndrom mit Bewusstseinsstörung. Kennzeichnend für das Delirium ist neben der Bewusstseinsstörung eine Störung der Aufmerksamkeit, der Wahrnehmung, des Denkens, der Kognition, des Gedächtnisses, der Psychomotorik und der Emotionalität. Pathognomonisch ist eine deutliche tageszeitliche Fluktuation der Symptome. Die akute psychische Störung hat entweder eine organische Ursache, oder entsteht aufgrund von Drogenwirkung oder Drogenentzug. Weitere Symptome sind Herabsetzung des abstrakten Denkvermögens, der Konzentration, ein eingeschränktes Kurzzeitgedächtnis und Desorientierung: Ein Betroffener ist nicht richtig orientiert, was Ort, Zeit, seine eigene Person oder Situation betreffen kann. Beim voll ausgeprägten Delirium kommt noch eine Störung des Schlaf-Wach-Rhythmus hinzu. Weitere Symptome, wie optische Halluzinationen, Wahnvorstellungen, motorische Unruhe und nestelnde Bewegungen sowie affektive Störungen wie Depression, Angst aber auch Euphorie oder Reizbarkeit und eine Agitation (krankhafte Unruhe) können auftreten. Der Beginn dieser akuten Störung ist plötzlich, die Symptomatik schwankt jedoch im Tagesverlauf. Die zwei Prägnanztypen sind hyperaktives und hypoaktives Delirium. Letzteres bietet mehr diagnostische Schwierigkeiten. Ebenso gibt es Mischformen mit Anteilen von beiden Typen. Unter Halluzination versteht man eine Wahrnehmung eines Sinnesgebietes, ohne dass eine nachweisbare Reizgrundlage vorliegt. Das bedeutet zum Beispiel, dass physikalisch nicht nachweisbare Objekte gesehen werden oder Stimmen gehört, ohne dass jemand spricht. Halluzinationen können alle Sinnesgebiete betreffen. Bei einer Illusion hingegen wird ein real vorhandener Sachverhalt verändert wahrgenommen: Ein tatsächlich vorhandener feststehender Gegenstand scheint sich zu bewegen oder in irregulären Mustern werden scheinbar Gesichter erkennbar. Bei optischen Halluzinationen kommt es zur Wahrnehmung nicht vorhandener Objekte. Am häufigsten sind kleine und bewegliche Objekte, deren Wahrnehmung dann meist sehr angstvoll erlebt wird. Dies kommt beispielsweise im Rahmen eines Deliriums vor. Bei akustischen Halluzinationen, die beispielsweise bei an Schizophrenie Erkrankten häufig sind, hören die Betroffenen oft imperative Stimmen. Cognitive Trajectories after Postoperative Delirium Delirium is common after cardiac surgery and may be associated with long-term changes in cognitive function. We examined postoperative delirium and the cognitive trajectory during the first year after cardiac surgery. We enrolled 225 patients 60 years of age or older who were planning to undergo coronary-artery bypass grafting or valve replacement. Patients were assessed preoperatively, daily during hospitalization beginning on postoperative day 2, and at 1, 6, and 12 months after surgery. Cognitive function was assessed with the use of the Mini–Mental State Examination (MMSE; score range, 0 to 30, with lower scores indicating poorer performance). Delirium was diagnosed with the use of the Confusion Assessment Method. We examined performance on the MMSE in the first year after surgery, controlling for demographic characteristics, coexisting conditions, hospital, and surgery type. Confusion Assessment Method (CAM; a diagnostic algorithm to determine the presence or absence of delirium on the basis of four features: acute change with a fluctuating course, inattention, disorganized thinking, and altered level of consciousness), and the Delirium Symptom Interview (an interview that assesses the presence or absence of eight features of delirium, including the four features of the CAM diagnostic algorithm). The 103 participants (46%) in whom delirium developed postoperatively had lower preoperative mean MMSE scores than those in whom delirium did not develop (25.8 vs. 26.9, P<0.001). Delirium is associated with a significant decline in cognitive ability during the first year after cardiac surgery, with a trajectory characterized by an initial decline and prolonged impairment. A Pooled Analysis of Vitamin D Dose Requirements for Fracture Prevention The results of meta-analyses examining the relationship between vitamin D supplementation and fracture reduction have been inconsistent. We pooled participant-level data from 11 double-blind, randomized, controlled trials of oral vitamin D supplementation (daily, weekly, or every 4 months), with or without calcium, as compared with placebo or calcium alone in persons 65 years of age or older. Primary end points were the incidence of hip and any nonvertebral fractures according to Cox regression analyses, with adjustment for age group, sex, type of dwelling, and study. Our primary aim was to compare data from quartiles of actual intake of vitamin D (including each individual participant's adherence to the treatment and supplement use outside the study protocol) in the treatment groups of all trials with data from the control groups. In conclusion, our data suggest that high-dose vitamin D supplementation (≥800 IU per day) may reduce the risk of hip fracture in persons 65 years of age or older, independently of type of dwelling, age, and sex. Furthermore, our data support a 25-hydroxyvitamin D level above 60 nmol per liter for the prevention of fractures. Shock-Wave Lithotripsy for Renal Calculi A 42-year-old man without a history of kidney stones had intermittent left flank pain for several weeks before being seen by his primary care doctor. Urinalysis revealed microhematuria. Computed tomography (CT) of the abdomen and pelvis without contrast enhancement identified a calcification 12 mm in diameter in the left renal pelvis, associated with mild hydronephrosis and a normal-caliber ureter. The attenuation coefficient of the stone was 790 Hounsfield units, and the skin-to-stone distance was 8.5 cm. He was referred to a urologist, who reviewed the CT scan and recommended treatment with extracorporeal shock-wave lithotripsy. Nephrolithiasis is a common condition, with a lifetime prevalence of approximately 13% in men and 7% in women in the United States. Total health care expenditures reached nearly $4.5 billion annually, and this figure increased to $5.3 billion when the indirect costs of lost workdays were included. European Association of Urology Urolithiasis Guideline Panel released comprehensive guidelines,45 recommending shock-wave lithotripsy as first-line therapy for non–lower-pole renal calculi less than 2 cm in diameter and for lower-pole renal calculi less than 1 cm in diameter. For larger stones in either location, percutaneous nephrolithotomy is the recommended primary treatment. For lower-pole stones between 1 and 2 cm in diameter without unfavorable anatomical factors or shock-wave–resistant stone composition, lithotripsy can be considered as an option for primary management. The patient described in the vignette has a stone with a size (less than 2 cm in diameter) and location (non–lower pole) that is considered to be favorable for treatment with shock-wave lithotripsy. Findings on CT imaging, including the attenuation coefficient (less than 1000 Hounsfield units) and the skin-to-stone distance (less than 10 cm), also predict a favorable outcome. Although the stone composition cannot be reliably predicted by means of current CT findings, and the patient did not previously have a stone with a known composition, the favorable findings on CT suggest that the stone will probably fragment well and that the risk of obstructive complications will be low. Bei diesem Verfahren benötigt der Patient keine Vollnarkose, in der Regel wird nur ein leichtes Schmerzmittel intravenös verabreicht, der Patient bleibt ansprechbar. Gegen den bei der Behandlung entstehenden Lärm (rund 3000 niedrigfrequente Impulse in 30 Minuten) bekommt der Patient einen Gehörschutz. Sehr oft kann diese Behandlung auch ambulant durchgeführt werden. Die Belastung für den Patienten ist gering und durch die gezielte Bündelung der Stoßwellen weniger schmerzhaft als bei den Geräten erster Bauart mit Badewanne. A 31-year-old woman who had been unable to eat or drink for the preceding week was admitted to the hospital. For the preceding 8 months she had had nausea, vomiting, and abdominal discomfort and several episodes of crampy epigastric pain with vomiting and intermittent chills and sweats, but no documented fevers. She also had loose, pale stools occasionally, but these episodes did not represent a notable change from her baseline. Gradually increasing fatigue, loss of appetite, and a recent weight loss of several kilograms were also reported. The patient's medical history included hypertension, obesity, and migraine headaches. She had undergone Roux-en-Y gastric bypass 5 years before presentation and subsequently lost approximately 45 kg (100 lb). Her weight had been stable for the past few years; her body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) was 33. She had undergone laparoscopic cholecystectomy 10 years before presentation. Her only medication was nifedipine, and she took a multivitamin on occasion. Intravenous fluids were administered (1 liter of 0.90% sodium chloride followed by a continuous infusion of 5% dextrose in a solution of 0.45% sodium. chloride). The hematocrit was 29.4%, with a mean corpuscular volume of 109 fl. The white-cell count was 9350 per cubic millimeter and her platelet count 432,000 per cubic millimeter. The aspartate aminotransferase level was 210 U per liter, alanine aminotransferase 44 U per liter, alkaline phosphatase 191 U per liter, total bilirubin 0.6 mg per deciliter (10.3 µmol per liter), albumin 3.3 g per deciliter, prothrombin time 13.6 seconds, and partial-thromboplastin time 33.8 seconds. Amylase and lipase levels were normal, and a serum test for beta human chorionic gonadotropin was negative. Abdominal computed tomography revealed a diffusely fatty liver, with focal sparing of the medial portion of the right lobe, and hepatomegaly, with a liver span of 26.5 cm; the spleen, measuring 14.2 cm, showed borderline enlargement. On the second hospital day, confusion, blurry vision, and vertigo developed abruptly. A repeat examination revealed impaired lateral gaze in both eyes and nystagmus on both horizontal and upward gaze, with a positive Romberg test. The patient was noted to have a wide-based, unsteady gait and was able to take only a few steps, with assistance from two people. Enlargement of the mammillary bodies is shown in an image obtained with fluid-attenuated inversion recovery sequencing (Panel A, arrow), and enhancement is shown in a T1weighted magnetic resonance image obtained after the administration of contrast material (Panel B). The patient was given 500 mg of thiamine intravenously on an emergency basis. Subsequent testing revealed low levels of whole-blood thiamine (45 nmol per liter; normal range, 80 to 150) and of serum folate (4.6 ng per milliliter [10.4 nmol per liter]; normal range, 5.3 to 9.9 ng per milliliter [12.0 to 22.4 nmol per liter]), copper (46 µg per deciliter [7.2 µmol per liter]; normal range, 80 to 155 µg per deciliter [12.6 to 24.4 µmol per liter]), zinc (57 µg per deciliter [8.7 µmol per liter]; normal range, 66 to 120 µg per deciliter [10.0 to 18.4 µmol per liter]), and 25hydroxyvitamin D (6 ng per milliliter [15 nmol per liter]; normal range, 25 to 80 ng per milliliter [62 to 200 nmol per liter]). Die Hand-Fuß-Mund-Krankheit – Synonyme: Hand-Fuß-Mund-Exanthem, Falsche Maul- und Klauenseuche – ist eine viral bedingte, weltweit vorkommende, hoch ansteckende und deshalb epidemisch auftretende Infektionskrankheit. Nach einer durchschnittlichen Inkubationszeit von drei bis sechs Tagen kommt es in der Regel zu einer Erkrankung mit hohem Fieber, vorübergehenden Allgemeinsymptomen und einem symmetrischen Hautausschlag (Exanthem) mit Bläschenbildung an den Händen, Füßen und einem Enanthem der Mundschleimhaut, das sich mit kurzlebigen Bläschen von vier bis acht Millimeter Durchmesser in der Mundhöhle, vor allem im Bereich der Zunge, des Gaumens und der Wangenschleimhaut äußert. Lippen, weicher Gaumen, Tonsillen und Pharynx bleiben frei bzw. sind selten betroffen. Diese Bläschen wandeln sich in seichte, schmierig belegte, schmerzhafte Erosionen (Aphthen). Die Veränderungen an Händen und Füßen treten gleichzeitig oder nur kurze Zeit später auf und sind vermehrt an den Streckseiten der Finger und Zehen oder deren Seitenflächen, aber auch den Fußsohlen (Fersen) und Handflächen zu beobachten. Hände und Füße können dabei einen stechenden / spannenden Schmerz und starken Juckreiz aufweisen. Diese Erkrankung wird durch eine Infektion mit Coxsackie- (Typ A 5, 9, 10, 16, B2, 5), Echo- (Typ 6) oder Enteroviren (Humanes Enterovirus 71) verursacht. Möglicherweise verlaufen bis zu 70 % der Infektionen asymptomatisch (inapparente Infektion). Autopsy Findings in Children with Hand, Foot, and Mouth Disease (etwa wie Maul und Klauenseuche) From May 2008 through July 2010, an epidemic of hand, foot, and mouth disease occurred in Guangxi, China. During the epidemic, some children died of progressive cardiorespiratory failure. Postmortem pathological examinations were performed for 14 patients. Reversetranscriptase–polymerase-chain-reaction assays of various specimens (throat swabs or stool samples) were performed to detect enterovirus 71, coxsackievirus A17, and pan-enterovirus messenger RNA. Assays for enterovirus 71 were positive in 12 patients. Assays to detect coxsackievirus A17 were positive in 1 patient, and assays to detect other enteroviruses were positive in 1 patient. Sections of brain-biopsy specimens were stained with hematoxylin and eosin. A photomicrograph at low magnification (Panel A) shows neuronal necrosis and softening in the brain stem (arrow), and higher magnification (Panel B) reveals the neuronophagia phenomenon (blue arrow) and colloid (black arrow) in the brain stem. A photomicrograph at low magnification (Panel C) shows perivascular cuffing in the brain stem (arrow). A view of the medulla oblongata at low magnification (Panel D) shows hemorrhage (arrow). A 68-year-old man complained of urinary frequency and hypogastric discomfort. He was a smoker and had hypertension. Digital rectal examination showed a painful prostate but he had no fever. Urine analysis showed a pyuria and a bacteriuria of enterococcus species. The patient was treated with amoxicillin. 2 days after his admission, he suddenly developed acute right flank pain with hypotension. (A) Axial non-contrast-enhanced MDCT of the abdomen showing retroperitoneal haematoma (asterisk) surrounding a fissured infrarenal abdominal aneurysm (arrowheads). Contrast-enhanced MDCT angiography in axial (B) and sagittal (C) reformation with maximum intensity projection algorithm; CT angiogram shows anterior rupture from the wall of the abdominal aortic aneurysm (arrow), with massive intraperitoneal bleeding (contrast extravasation). Proprotein convertase subtilisin/kexin type 9, also known as PCSK9, is an enzyme which in humans is encoded by the PCSK9 gene. The encoded protein is synthesized as a soluble zymogen that undergoes autocatalytic intramolecular processing in the endoplasmic reticulum. The protein may function as a proprotein convertase. This protein plays a major regulatory role in cholesterol homeostasis. PCSK9 binds to the epidermal growth factor-like repeat A (EGF-A) domain of the low-density lipoprotein receptor (LDLR), inducing LDLR degradation. Reduced LDLR levels result in decreased metabolism of low-density lipoproteins, which could lead to hypercholesterolemia. Alnylam Pharmaceuticals has recently shown, in initial clinical trials, positive results of ALN-PCS, which acts by means of RNA interference, as an effective means of PCSK9 inhibition. Mutations in this gene have been associated with a rare form of autosomal dominant familial hypercholesterolemia (HCHOLA3). The mutations appear to cause the disease by increasing its protease activity, reducing LDL receptor levels and thereby preventing the uptake of cholesterol into the cells. Effect of a monoclonal antibody to PCSK9, to reduce low-density lipoprotein cholesterol in patients with heterozygous familial hypercholesterolaemia on stable statin dose with or without ezetimibe therapy: a phase 2 trial Inhibition of proprotein convertase subtilisin/kexin type 9 serine protease (PCSK9) resulted in large reductions of low-density lipoprotein cholesterol (LDL-C) in phase 1 trials. We assessed the efficacy and safety of various doses and dosing intervals of REGN727, a monoclonal antibody to PCSK9, added to statins, to further lower LDL-C in patients with heterozygous familial hypercholesterolaemia. This multicentre, randomised, placebo-controlled phase 2 trial was done at 16 lipid clinics, we enrolled adults with heterozygous familial hypercholesterolaemia and LDL-C concentrations of 2·6 mmol/L or higher on stable diet and statin dose, with or without ezetimibe. Patients were randomly assigned to receive REGN727 150 mg, 200 mg, or 300 mg every 4 weeks, or 150 mg every 2 weeks, or placebo every 2 weeks (ratio 1:1:1:1:1). Randomisation was stratified by concomitant use of ezetimibe at baseline. Investigators, study staff, and patients were masked to treatment group. Blinding was maintained by administration of placebo alternating with REGN727 for the groups of 4 week dosing. The primary endpoint was mean percent reduction in LDL-C from baseline at week 12 and was analysed in the modified intention-to-treat population with an analysis of covariance (ANCOVA) model with treatment group. REGN727 was well tolerated and achieved substantial further LDL-C reduction in patients with heterozygous familial hypercholesterolaemia and elevated LDL-C treated with high-dose statins, with or without ezetimibe. REGN727 has the potential to provide optimum control of LDL-C in patients with this disorder. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study Long-term disorders are the main challenge facing health-care systems worldwide, but health systems are largely configured for individual diseases rather than multimorbidity. We examined the distribution of multimorbidity, and of comorbidity of physical and mental health disorders, in relation to age and socioeconomic deprivation. In a cross-sectional study we extracted data on 40 morbidities from a database of 1 751 841 people registered with 314 medical practices in Scotland as of March, 2007. We analysed the data according to the number of morbidities, disorder type (physical or mental), sex, age, and socioeconomic status. We defined multimorbidity as the presence of two or more disorders. Our findings challenge the single-disease framework by which most health care, medical research, and medical education is configured. A complementary strategy is needed, supporting generalist clinicians to provide personalised, comprehensive continuity of care, especially in socioeconomically deprived areas. Magnesium for aneurysmal subarachnoid haemorrhage (MASH-2): a randomised placebo-controlled trial Magnesium sulphate is a neuroprotective agent that might improve outcome after aneurysmal subarachnoid haemorrhage by reducing the occurrence or improving the outcome of delayed cerebral ischaemia. We did a trial to test whether magnesium therapy improves outcome after aneurysmal subarachnoid haemorrhage. We did this phase 3 randomised, placebo-controlled trial in eight centres in Europe and South America. We randomly assigned (with computergenerated random numbers, with permuted blocks of four, stratified by centre) patients aged 18 years or older with an aneurysmal pattern of subarachnoid haemorrhage on brain imaging who were admitted to hospital within 4 days of haemorrhage, to receive intravenous magnesium sulphate, 64 mmol/day, or placebo. We excluded patients with renal failure or bodyweight lower than 50 kg. Patients, treating physicians, and investigators assessing outcomes and analysing data were masked to the allocation. The primary outcome was poor outcome—defined as a score of 4—5 on the modified Rankin Scale—3 months after subarachnoid haemorrhage, or death. We analysed results by intention to treat. We also updated a previous meta-analysis of trials of magnesium treatment for aneurysmal subarachnoid haemorrhage. The MASH 2 trial has implications for clinical practice. Administration of magnesium after aneurysmal subarachnoid haemorrhage is standard practice in many centres. On the basis of the results of MASH 2—a trial of treatment of aneurysmal subarachnoid haemorrhage with sufficient power to detect a clinically significant improvement in outcome—and in combination with data from other trials, we do not recommend routine use of intravenous magnesium 64 mmol/day for the improvement of outcome after aneurysmal subarachnoid haemorrhage. The 10/66 Dementia Research Group is a collective of researchers carrying out populationbased research into dementia, non-communicable diseases and ageing in low and middle income countries.10/66 refers to the two-thirds (66%) of people with dementia living in low and middle income countries, and the 10% or less of population-based research that has been carried out in those regions.10/66 is a part of Alzheimer's Disease International, and is coordinated from the Institute of Psychiatry, King's College London. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). DSM-IV manual is published by the American Psychiatric Association and covers all mental health disorders for both children and adults. It also lists known causes of these disorders, statistics in terms of gender, age at onset, and prognosis as well as some research concerning the optimal treatment approaches. Mental Health Professionals use this manual when working with patients in order to better understand their illness and potential treatment and to help 3rd party payers (e.g., insurance) understand the needs of the patient. The book is typically considered the ‘bible’ for any professional who makes psychiatric diagnoses in the United States and many other countries. Much of the diagnostic information on these pages is gathered from the DSM IV. Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve Results of the few cohort studies from countries with low incomes or middle incomes suggest a lower incidence of dementia than in high-income countries. We assessed incidence of dementia according to criteria from the 10/66 Dementia Research Group and Diagnostic and Statistical Manual of Mental Disorders (DSM) IV, the effect of dementia at baseline on mortality, and the independent effects of age, sex, socioeconomic position, and indicators of cognitive reserve. We did a population-based cohort study of all people aged 65 years and older living in urban sites in Cuba, the Dominican Republic, and Venezuela, and rural and urban sites in Peru, Mexico, and China, with ascertainment of incident 10/66 and DSM-IV dementia 3—5 years after cohort inception. We used questionnaires to obtain information about age in years, sex, educational level, literacy, occupational attainment, and number of household assets. We obtained information about mortality from all sites. For participants who had died, we interviewed a friend or relative to ascertain the likelihood that they had dementia before death. In this study of more than 12 800 individuals, incidence rates for 10/66 dementia were roughly 1·5 —2·5 times higher than those for DSM-IV dementia. Mortality hazards were higher in individuals with dementia at baseline than in dementia-free individuals. Informant reports suggested a high incidence of dementia before death; overall incidence could be between 4% and 19% higher if these data were included. 10/66 dementia incidence was independently associated with increased age, female gender, and low education, but not with occupational attainment. Our results provide supportive evidence for the cognitive reserve hypothesis, showing that in middle-income countries as in high-income countries, education, literacy, verbal fluency, and motor sequencing confer substantial protection against the onset of dementia. Sport and exercise as contributors to the health of nations Self-reported rates of participation in sport vary by country. In the UK, about 40% of men and women aged 16 years or older participate in at least one sport every week. Although few data exist to assess trends for participation in sport, there is little evidence of change in the past decade among adults. Large cohort studies suggest that such participation in sport is associated with a 20 —40% reduction in all-cause mortality compared with non-participation. Randomised trials and crossover clinical studies suggest that playing sport is associated with specific health benefits. Some sports have relatively high injury risk although neuromuscular training programmes can prevent various lower extremity injuries. Clinicians can influence a large number of patients through brief interventions that promote physical activity, and encouragement toward participation in sport for some physically inactive patients qualifies as evidence-based therapy. Exercise might also be considered as a fifth vital sign and should be recorded in patients' electronic medical records and routine histories. Sport, exercise, and physical activity (A) Domains of sport, exercise, and physical activity. (B) Individual who exercises and plays sport but is otherwise sedentary. (C) Physically active individual who does no explicit sport or exercise. 39-year-old woman presented complaining of a 1-day history of vomiting and abdominal pain. She had had three or four episodes, with no infective prodrome. She was a physiotherapist and a competent long-distance runner; 2 days earlier she had run a 5 km race, and that morning had done her daily exercise workout. On examination there were no physical signs other than sinus tachycardia. Within 2 h, she collapsed and was moribund in acute cardiogenic shock. Chest radiography showed pulmonary congestion. Transthoracic echocardiography showed a slightly dilated, poorly functioning heart with no pericardial effusion. Cardiac catheterisation was done to exclude coronary artery disease, and an intra-aortic balloon pump was placed for circulatory support. She had no arrhythmias. Acute myocarditis was suspected and she was transferred to our cardiothoracic centre. She arrived 8 h after first presentation, was found to be in extremis, with fixed mottling of her trunk and limbs and hypotension despite epinephrine infusing at >1 µg/kg per min. She was anuric, profoundly acidaemic, and hypoxic on 100% oxygen (PaO2 6·1 kPa, pH 6·9, lactate 16 mmol/L, base excess −13). The heart was tense and dilated and a myocardial biopsy sample was taken from the left ventricle. Central veno-arterial extracorporeal membrane oxygenation (ECMO) was established; a cannula was inserted via the abdominal wall into the right atrium to drain systemic venous blood into the ECMO pump, which returned oxygenated blood via a separate cannula into the ascending aorta CT of the abdomen showed a large left adrenal mass (5×6 cm). Left adrenalectomy was done (day 3) with concurrent ECMO support. Subsequent echocardiography showed recovering biventricular function (day 5) and ECMO was discontinued. Myocyte necrosis with contraction bands, perivascular edema, and microvascular endothelial swelling with no evidence of myocarditis. Immunohistochemical staining for C4d was strongly positive along the microvasculature and in rare individual myocytes with contraction band injury Hematoxylin & eosin, 10X. Myocardium with coagulative myocyte necrosis in center and lower right corner.