Onkologische Aspekte - Tumorzentrum Berlin-Buch
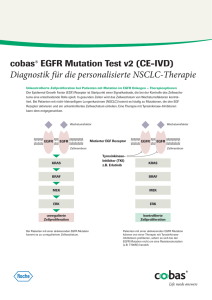
Werbung

Aktuelle Therapieoptionen im Stadium IIIB/IV des Lungenkarzinom Tumorzentrum Berlin - Buch 13.1. 2016 Ansatzpunkte zur Aktivierung des Immunsystems Stimulierende und inhibierende Faktoren des Tumor-Immunitäts-Zyklus 3 Priming und Aktivierung Trafficking von T-Zellen zu Tumoren CD28/B7.1, CD137/CD137L OX40/OX40L, CD27/CD70 HVEM, GITR, IL-2, IL-12 CX3CL1, CXCL9, CXCL10, CCL5 CTLA4/B7.1, PDL1/PD-1 PD-L1/B7.1 2 Tumor Erkennung von Tumorzellen durch T-Zellen Chen and Mellman, Immunity. 2013 Jul 25; 39(1): 1 6 T-Zell Rezeptor Verringerte pMHC auf Tumorzellen Freisetzung von Tumorzell-Antigenen Immunogener Zelltod Tolerogener Zelltod 5 LFA1/ICAM1, Selectins VEGF, Endothelin-B Rezeptor Tumor-Antigen Präsentation TNF-, IL-1 IFN-, CD40L/CD40 CDN, ATP HMGB1, TLR IL-10, IL-4, IL-13 1 Infiltration von T-Zellen in Tumore Blood vessel Lymphknoten 4 Zerstörung von Tumorzellen IFN- , T-Zell-Granulat Inhalt PD-L1/PD-1 PD-L1/B7.1 IDO TGF- BTLA VISTA 7 LAG-3 Arginase MICA/MICB B7-H4 TIM3/Phospholipide 3 Blockade der CTLA-4- und PD-1- Signalwege Mikroumgebung des Tumors Lymphknoten Aktivierung (Zytokine, Lyse, Proliferation, Migration zum Tumor) MHC TCR TCR Dendritische B7 CD28 Zelle B7 CTLA-4 Anti-CTLA-4 +++ +++ +++ T-Zelle --- MHC T-Zelle --- PD-1 PD-L1 Tumorzelle Anti-PD-1/PD-L1 --- PD-1 PD-L2 Anti-PD-1 CTLA-4 Signalweg CTLA-4 reguliert die Amplitude der frühen Aktivierung von naiven und Memory T-Zellen. PD-1 Signalweg PD-1 begrenzt die T-Zell-Aktivierung in der Peripherie während einer Entzündungsreaktion. Wolchock et al, J Clin Oncol 2013 ASCO Abstracts 31:15 4 CA184-041: Phase II trial to evaluate Ipilimumab in combination with chemotherapy (carboplatin/paclitaxel) in lung cancer (NSCLC and SCLC): Immunrelated progression free survival of concurrent and phased regimen 0.8 Control Concurrent Ipilimumab 0.6 Events/ patients 56/66 55/70 0.4 0.2 0 0 No. at risk Control Ipilimumab 2 4 6 8 10 12 Time (months) 66 59 55 41 38 28 17 13 11 5 70 62 48 44 40 34 29 20 18 9 4 8 3 6 3 2 14 3 1 1 1 1 0 1 0 irPFS (probability) 0.6 0.4 0.2 0 0 2 4 6 8 10 12 14 16 Time (months) 0.6 0.4 0.2 0 2 4 18 20 22 No. at risk Control 45 44 42 38 36 26 11 10 7 5 4 3 2 2 2 2 1 0 0 0 0 0 0 0 Ipilimumab 43 38 36 31 29 26 16 12 11 10 9 9 8 5 4 3 3 2 2 2 2 2 1 0 6 8 10 12 Time (months) No. at risk Control 66 59 55 41 38 28 17 13 11 5 Ipilimumab 66 59 55 41 38 28 17 13 11 5 ED-SCLC (Phased) Median Events/ OS, P patients months 95% CI HR value 4,67– Control 40/45 5,26 5,72 Concurrent 5,19– 0,7 37/43 5,68 0,11 Ipilimumab 6,87 5 0.8 0.8 0 0 0 Median Events/ OS, P patients months 95% CI HR value 4,14– Control 56/66 4,63 5,52 Phased 4,76– 0,7 54/68 5,68 0,05 Ipilimumab 7,79 2 1.0 16 ED-SCLC (Concurrent) 1.0 NSCLC (Phased) irPFS (probability) 1.0 Median OS, P months 95% CI HR value 4,63 4,14–5,52 0,8 5,52 4,17–6,74 0,13 1 irPFS (probability) irPFS (probability) NSCLC (Concurrent) 1.0 0.8 0.6 4 4 3 3 3 3 14 3 3 1 1 16 1 1 1 1 0 0 Median Events/ OS, P patients months 95% CI HR value 4,67– Control 40/45 5,26 5,72 Phased 5,29– 0,6 38/42 6,44 0,03 Ipilimumab 7,75 4 0.4 0.2 0 0 2 4 6 8 10 12 14 Time (months) 16 18 20 22 No. at risk Control 45 44 42 38 36 26 11 10 7 5 4 3 2 2 2 2 1 0 0 0 0 0 0 Ipilimumab 42 42 40 37 35 31 22 18 10 7 7 6 6 6 5 5 5 3 2 1 1 1 0 Data from trial CA184-041.; a Statistically significant per protocol-stipulated one-sided α=0.1; P values not adjusted for multiple comparisons.; HR = hazard ratio; Ipi = ipilimumab; irPFS = PFS by immune-related response criteria (irRC); mWHO-PFS = PFS by modified WHO criteria (mWHO); Pbo = placebo; PFS = progression-free survival; Lynch et al, J Clin Oncol. 2012; 30: 2046; Reck et al, Ann Oncol. 2013; 24: 75 5 Remission unter Therapie Ausgewählte Biomarker-Ansätze für Immunonkologische Therapien 1. Expression von Markern bezogen auf das Ziel-Molekül oder den Ziel-Signalweg z. B. PD-L1 für PD-1-Signalweg gerichete Therapien1 2. Therapiebedingte Veränderungen des Immunsystems oder der Tumorumgebung („Microenvironment”) z. B. absolute Lymphozytenzahl (ALC)2, Antikörperantwort auf Tumorantigene3 oder Veränderung der Tumor-infiltrierenden Lymphozyten (TIL)4 3. Genexpressionsprofil des Patienten oder des Tumors z. B. differenzielle Expression des Tumors von immunologischen Genen5 1. Callahan et al, J Clin Oncol 2013; 31(15 Suppl): abstract 3003; 2. Ku et al, Cancer 2010; 116: 1767; 3. Postow et al, N Engl J Med 2012; 366(10): 925; 4. Hamid et al, J Transl Med 2011; 9: 204; 5. Ulloa-Montoya et al, J Clin Oncol 2013; 31: 2388 8 KEYNOTE-001: Response Rate by Level of PD-L1 Expression (RECIST v1.1, Central Review) • Clinical trial assay – Strong PD-L1 expression: defined as ≥50% membranous staining in tumor cells – Weak PD-L1 expression: defined as 1–49% membranous staining in tumor cells Garon et al, Oral presentation at ESMO 2014 10 CA209-003 NSCLC cohort: Change in tumour burden according to EGFR and KRAS mutation status: example with Nivolumab (anti-PD-1) in NSCLC Change in tumour size (%) 100 80 60 120 EGFR mutation status Mutant 100 Unknown WT 40 20 0 –20 –40 –60 Change in tumour size (%) 120 80 60 KRAS mutation status Mutant Unknown WT 40 20 0 –20 –40 –60 –80 –80 –100 –100 Patients Patients Dashed horizontal lines denote 30% decrease for PR (in the absence of new lesions) and 20% increase for PD per RECIST v1.0 Nivolumab demonstrates responses across a broad array of NSCLC patient populations regardless of the KRAS or EGFR mutational status Adapted from Gettinger et al, Poster presentation at WCLC 2013. J Thorac Oncol. 2013; 8(suppl 2): abstract: P2.11-038 11 Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2015 Dec 18. pii: S0140-6736(15)01281-7. doi: 10.1016/S0140-6736(15)01281-7. [Epub ahead of print] KEYNOTE-001: Summary of Exposure and Treatment-Related-AEs • Infusion-related reactions occurred in 4 patients (1,5%) • Other potentially immune-mediated AEs that occurred in <1% of patients were colitis and hyponatremia Garon et al, Oral presentation at ESMO 2014 18 CA209-003: Response by smoking exposure according to RECIST response in NSCLC patients treated with nivolumab 50 0 -50 -100 Patients 100 50 0 -50 -100 Patients Nivolumab (NSCLC-Cohort) 100 >5 pack-yrs smokers Change From Baseline (%) Change From Baseline (%) ≤5 pack-yrs smokers PD = progressive disease PR = partial response SD = stable disease Hellmann et al, Poster presentation at ESMO 2014 19 CA209-003: Response by smoking exposure in NSCLC patients treated with nivolumab Variable ORR, % (n/N) [95% CI] P-value Smoking exposure ≤5 pack-yrs 0 (0/14) [0, 23] >5 pack-yrs 30 (20/66) [20, 43] 0,018 Time since quitting 0/never smoker 0 (0/10) [0, 31] Current smoker 27 (6/22) [11, 50] 1–5 yrs prior 46 (6/13) [19, 75] 6–15 yrs prior 17 (2/12) [2, 48] >15 yrs prior 26 (6/23) [10, 48] 0,12 • Among smokers, there was no association between ORR and time since quitting • The impact of smoking in squamous lung cancers could not be assessed, as there was only one non-smoker among patients with squamous lung cancers Subgroup Nivolumab 3 or 10 mg/kga ≤5 pack-yrs • ORR was significantly higher in >5 pack-yrs smokers compared with ≤5 pack-yrs smokers; this differential response rate was numerically more pronounced in the subgroup receiving 3 mg/kg or higher and remained true in the adenocarcinoma-only cohort 0 (0/10) [0, 31] 0,023 >5 pack-yrs 37 (19/52) [24, 51] Adenocarcinoma ≤5 pack-yrs 0 (0/13) [0, 25] 0,049 >5 pack-yrs 25 (8/32) [11, 43] 20 CA209-003: Conclusion NSCLC cohort NSCLC cohort (n=129) Nivolumab demonstrates responses across a broad array of NSCLC patient populations regardless of histology, including populations of more heavily pretreated patients (≥3 prior approximately), older patients (age ≥70 years old) and patients with and without tumors driven by KRAS or EGFR mutations Nivolumab activity was numerically higher in the PD-L1 positive patients, but PD-L1 negative patients also exhibited overall responses A history of smoking was significantly associated with improved response and PFS to nivolumab Hodi et al, Poster presentation at ECC 2013: abstract 880 21 Unterschiedliches Nebenwirkungsprofil onkologischer Therapien Chemotherapie I-O Therapien Zielgerichtete Therapien Ziel Sich schnell teilende Tumorzellen und normale Zellen Ziel Immunsystem Ziel Spezifische Moleküle, die in Tumorwachstum involviert sind Nebenwirkungen Divers aufgrund unspezifischer Therapie Nebenwirkungen Einzigartige NW aufgrund der Aktivierung des Immunsystems Nebenwirkungen Spiegeln die Rolle des Targets wider Unterschiedliches Spektrum an Nebenwirkungen Manche NW unter I-O Therapien ähneln den NW der anderen Therapien ABER – NW können unterschiedliche Ursachen haben Beispiele: Diarrhö/Kolitis, Fatigue, Rash/Juckreiz, Endokrinopathien Andere Strategien zum NW-Management notwendig Topalian et al, N Eng J Med 2012; 366(26): 2443 oral presentation at ASCO 2013: J Clin Oncol 2013; 31(15 suppl): abstract 3002; Hamid et al, N Eng J Med 2013; 369: 134; 22 Management of acquired resistance to epidermal growth factor receptor kinase inhibitors in patients with advanced non-small cell lung cancer Cancer Volume 120, Issue 15, pages 2289-2298, 17 APR 2014 Distribution of the 60 rare EGFR mutations The Oncologist 2015;20:1–8 Time to treatment failure of common and uncommon EGFR mutations The Oncologist 2015;20:1–8 Management of acquired resistance to epidermal growth factor receptor kinase inhibitors in patients with advanced non-small cell lung cancer Cancer Volume 120, Issue 15, pages 2289-2298, AZD9291 in EGFR Inhibitor–Resistant Non–Small-Cell Lung Cancer Best Percentage Change in Target-Lesion Size. Jänne PA et al. N Engl J Med 2015;372:1689-1699. Best Response to Rociletinib. Sequist LV et al. N Engl J Med 2015;372:1700-1709. Management of acquired resistance to epidermal growth factor receptor kinase inhibitors in patients with advanced non-small cell lung cancer Cancer Volume 120, Issue 15, pages 2289-2298, Die Biopsie ist Grundlage einer erfolgreichen Bestimmung des EGFR-Mutationsstatus • Vorab zu klären: Wie kann das tumorhaltige Material am besten gewonnen werden? (endoskopisch, perkutan etc.) • Falls erforderlich: Rücksprache, wie das Material zum Pathologen versendet werden soll • Zu beachten/Empfehlung: Immer 4 bis 5 Biopsien pro Läsion • Wenn möglich: Unterschiedliche Areale der Läsion biopsieren • Neben dem Primärtumor ggf. auch Metastasen biopsieren Mechanismen zur Freisetzung von Tumorzell-DNA in den Blutkreislauf – Absterben von Tumorzellen durch Nekrose oder Apoptose 1. Pathak, AK et al. Clinical Chemistry 2006; 52: 1833–1842. 2. Gormally, E et al. Mutation Research 2007; 635: 105–117. 3. Aung, KL et al. The HUGO Journal 2010; 4: 11–21. Mechanismen zur Freisetzung von Tumorzell-DNA in den Blutkreislauf – Spontane und aktive Sekretion von DNA aus den Tumorzellen in die Zirkulation 1. Pathak, AK et al. Clinical Chemistry 2006; 52: 1833–1842. 2. Gormally, E et al. Mutation Research 2007; 635: 105–117. 3. Aung, KL et al. The HUGO Journal 2010; 4: 11–21. ctDNA-Testung – von der Probe zur Analyse • Plasma eignet sich am besten für die ctDNA-Isolation • Aus 10ml Vollblut können etwa 5ml Plasma gewonnen werden • Zur Maximierung des Testerfolgs sollte das größtmögliche Volumen gewählt werden. Abnahme des peripheren Blutes im Plasmaröhrchen (mind. 10 ml) Abpipettieren des Plasmas bis 0,5 cm oberhalb der festen Blutbestandteile Aufteilen des gewonnenen Plasmas (2–5 ml) auf Kryoröhrchen Zentrifugation des Plasmaröhrchens für 10 min bei 4°C und 2000 g Tieffrieren des Plasmas nach Möglichkeit auf Trockeneis Versand des Plasmas auf Trockeneis an das molekularpathologische Labor Durchführung der DNA-Extraktion und anschließende EGFR-Mutationsanalyse Assess Study design Objectives Primary Patients • Patients with newly diagnosed, locally advanced/metastatic chemotherapy-naïve NSCLC not suitable for curative treatmenta or • Recurrent disease and surgical resection with / without adjuvant chemotherapy • Concordance between EGFR mutation status obtained via tissue / cytology and blood (plasma) based testing Secondary • EGFR mutation frequency Samples • Provision of tumour and plasma samples for EGFR mutation testing Assessments Tissue / cytologyb • Correlations between EGFR mutation status and demographic data / disease status • EGFR mutation testing according to local practices following histopathological review (WHO classification) • EGFR mutation testing practices Blood (plasma)b • 1st-line therapy (all patients) • Samples processed to plasma and transported to designated laboratories for EGFR mutation testing • 2nd-line therapy (patients with EGFR mutation-positive NSCLC) EGFR mutation frequency ADC non-ADC n/N (%) n/N (%) Japan 78/195 (40.0) 6/77 (7.8) Europe 99/712 (13.9) 6/180 (3.3) Japan 40 (51.3) - Europe 54 (54.5) - Japan 37 (47.4) - Europe 28 (28.3) - Japan 0 (0) - Europe 1 (1.0) - Japan 0 (0) - Europe 4 (4) - Japan 1 (1.3) - Tissue / cytology Overall EGFR mutationpositive % (n=189) • Female gender, ADC histology, never-smoking status, and Japanese ethnicity significantly correlated with EGFR mutation-positive tissue/cytology and plasma sample (all p<0.1) • There was a trend between increasing number of metastases and EGFR mutation-positive plasma sample (p=0.054) • Immunohistochemistry analyses showed that 4.3% (10 / 231) of TTF-1negative tissue / cytology samples were EGFR mutation-positive – Exon 19 del (n=4), L858R (n=4), G719X (n=1), S768I & V769L (n=1) Subtype (% of overall positive)a Exon 19 deletion L858R only T790M + other Exon 20 insertion - Serial measurement of plasma genotype for disease monitoring. Geoffrey R. Oxnard et al. Clin Cancer Res 2014;20:16981705 ADAURA Trial Design •Phase III, double-blind, randomized, placebo-controlled study •Assess the efficacy and safety of AZD9291 vs placebo in patients with stage IB-IIIA NSCLC with centrally confirmed, common sensitising EGRF mutations (Ex19Del of L858R) who have had complete tumour resection, with or without postoperative adjuvant chemotherapy Stage IB– IIIA EGFRm+ NSCLC (Ex19del or L858R) No adjuvant chemo Physician choice (N~700) 1:1 Randomization Complete Adjuvant surgical •Estimated of 700 patients resectionEnrolment chemo 37 DFS: disease free survival; OS: overall survival; * Initial dose of 80mg QD can be reduced to 40mg QD NCT02511106 Accessed 22 September 2015 Stratification: (stage, race, mutation type) AZD9291 80mg* QD 3 years of treatment Placebo Endpoints: 1ry: DFS 2ry: OS Vielen Dank 1744204/12