An amorous adventure with side effects
Werbung
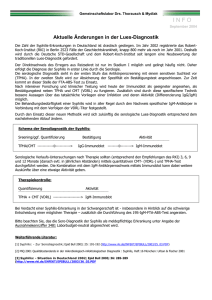
Schlussfolgerung: Das Auftreten der FSME beginnt in der Regel im März mit einem Häufigkeitsgipfel von Juni bis August und Einzelfällen bis November. Typisch ist ein zweiphasiger Verlauf nach einer bis zu zehntägigen Inkubationszeit. Durch die Virämie kommt es zu Grippesymptomen, die nach wenigen Tagen wieder abklingen. Nach einem symptomfreien Intervall von 1 bis 10 Tagen treten die neurologischen Symptome der Meningoenzephalitis auf. Das Übertragungsrisiko einer FSME beträgt etwa 30%. Während die Infektion in nur etwa 1% der Fälle letal verläuft, leiden 50% der Patienten nach 6 Monaten noch unter Restbeschwerden, bei 30% der Patienten persistieren Langzeitresiduen. Besonderheiten des beschriebenen Falles sind einerseits die zeitliche Nähe zum operativen Eingriff, welcher im beschwerdefreien Intervall stattfand, andererseits die nicht ganz typische Jahreszeit. Auch im Spätherbst treten allerdings noch FSME-Infektionen auf. Der beschriebene Fall führt einmal mehr die Relevanz der FSME-Impfung im Endemiegebiet und bei entsprechender Exposition vor Augen. P335 An amorous adventure with side effects C. Bocion, V. Nagy, P.E. Ballmer, U. Karrer, B. Rodic Cantonal Hospital Winterthur (Winterthur) Introduction: A 59-year-old man developed bilateral facial nerve palsy, progressive hearing loss, axillary lymphadenopathy, and a macular rash on the trunk. He reported unprotected sexual intercourse with a female hotel employee in Thailand five weeks ago, and recalled a similar rash on her belly. Results: Serologic blood testing revealed a positive Treponema pallidum Hemagglutination (TPHA) of 1280 and a Veneral Disease Research Laboratories (VDRL) test of 2. Human immunodeficiency virus (HIV) screening was negative. Cerebrospinal fluid (CSF) analysis showed a slight pleocytosis (6/mcL), and normal values for protein, lactate, and albumin. Oligoclonal bands were positive, and an unspecific alteration of the blood-brain-barrier was described. VDRL in the CSF was negative and TPHA was negative, indicating the absence of significant intrathecal antibody production. MRI was consistent with neurosyphilis with bilateral involvement of the facial nerve. After corticosteroid prophylaxis of a Herxheimer reaction, the patient was treated with 6 x 3 million units of penicillin G intravenously for 14 days. Hearing and facial nerve function improved. Conclusion: Syphilis is a sexually transmitted disease caused by the spirochete Treponema pallidum. Syphilis presents with four clinical stages, and the involvement of the central nervous system may be present from weeks to many years after infection (stages II to IV). Within two to four weeks after occurrence of primary chancre, secondary syphilis may develop, which can be associated with rash, lymphadenopathy and occasional aseptic meningitis. If neurologic symptoms are present, CSF examination is mandatory. In case of characteristic clinical findings and response to appropriate antibiotic treatment, neurosyphilis may be diagnosed even in the absence of a positive VDRL test in CSF. Any stage of syphilis should be treated with parenteral penicillin to avoid disease progression and transmission. The exact dose and regimen depend on the disease stage and the immune status of the patient. Neurosyphilis should be treated intravenously. Follow up serologic testing at 3, 6, and 12 months should demonstrate a decline in VDRL titer, indicating an adequate response to treatment. As the prevalence of syphilis increases worldwide, early complications of neurosyphilis are getting more frequent, and should be considered in diagnostic evaluation of abnormal neurologic conditions. P336 Neurocysticercosis - a rare cause of epilepsy in Switzerland F. Lüscher (1), G. Laifer (1), S. Dinges (1), C.A. Meier (1), K. Nedeltchev (1), C. Beynon (1), C. Hatz (2), A. Schibli (1) (1)Stadtspital Triemli (Zürich); (2)Swiss Tropical and Public Health Institute (Basel) Background: Cysticercosis is caused by the larval stage of the pork tapeworm Taenia solium. In developing countries neurocysticercosis (NCC) is the most common parasitic disease of the central nervous system and an important reason for acquired adult-onset seizures. Case report: A 37-year-old man from Switzerland was admitted for a first episode of a generalized seizure. He had a history of meningitis 17 years ago but reported no use of illicit drugs, head trauma or family history of epilepsy. During the past 15 years he had travelled several times to South America and Southeast Asia. Physical examination, a complete blood count and CRP were normal. Cranial CT revealed a frontal cystic enhancing lesion with perifocal edema (fig. 1) and several calcified small lesions. Examination of the cerebrospinal fluid was normal. Due to the clinical and radiographic presentation, NCC was suspected and confirmed by EITB for Taenia solium. He was treated with